Affiliate Disclaimer
Some links in this article are affiliate links. We may earn a small commission if you make a purchase through these links, at no extra cost to you. We only recommend products we find useful to our readersAn uncommon yet deadly cancer that starts in the vaginal tissues is called vaginal cancer. Even though vaginal cancer is uncommon, knowledge about it is essential because of the possible effects it may have on women’s health. Early identification significantly increases the likelihood that treatment and recovery will be successful. This article explores 10 prominent causes of vaginal cancer and clarifies the different risk factors that lead to the development of this disease. We hope to educate women, promote preventative health measures, and improve the prognosis for individuals impacted by this disease by raising awareness and advocating for early detection.
What is vaginal cancer?
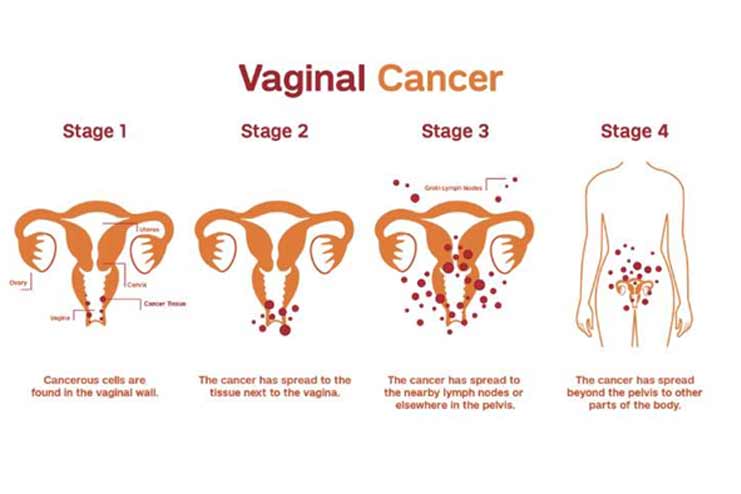
A malignant tumor that starts in the vaginal tissues and frequently affects the vaginal epithelial cells is called vaginal cancer. Adenocarcinoma and the squamous cell carcinoma are the two main ways it manifests. About 85% of cases of carcinoma are of the most common kind, squamous cell carcinoma, which originates from the thin, flat cells lining the vagina. Less frequently occurring adenocarcinomas begin in the epithelial cells that line the vagina.
Although only making up about 1% to 2% of all gynecological cancers, vaginal cancer is more common in older adults, primarily affecting women over the age of 60. A history of cervical cancer, an infection with the human papillomavirus (HPV), and prolonged exposure to diethylstilbestrol (DES) during pregnancy are additional risk factors. Early detection and effective treatment are contingent upon awareness of these risk factors and demographic trends to lower the overall incidence and improve the prognosis for affected women.
Symptoms of Vaginal Cancer
In many cases, the signs and symptoms of vaginal cancer are not immediately apparent. These symptoms can include abnormal vaginal bleeding, particularly after sexual activity or menopause, atypical vaginal discharge, a palpable tumor or lump in the vagina, pain during sexual activity, and pelvic pain. There may be problems with the urinary system, such as experiencing pain or difficulties when peeing.
The diagnosis of these symptoms at an early stage is necessary for effective treatment. Diagnosing vaginal cancer at an earlier stage significantly improves the prognosis and treatment outcomes. As a result, it is of the utmost importance for women to remain watchful regarding any changes that may occur in their vaginal health and to seek medical assistance as soon as possible if they see any symptoms that are not typical. Early detection can also be aided by routine gynecological screenings and check-ups, such as Pap smears, which can be performed even before manifestations of the disease become apparent. Increased awareness and preventive health practices can significantly lower the risks of vaginal cancer, which can also result in more favorable cancer treatment outcomes.
10 Causes of Vaginal Cancer
Human Papilloma Virus: Infection with the human papillomavirus (HPV) is a significant cause of squamous cell carcinoma. There are various strains of HPV, a sexually transmitted disease, some of which are high-risk and linked to the development of cancer. The virus alters the vaginal cells, resulting in aberrant growths that have the potential to develop into cancer over time. If left untreated, precancerous lesions from a persistent HPV infection may develop into vaginal cancer.
HPV-related vaginal cancer is more common in women with a compromised immune systems, such as those living with HIV. Frequent screenings are essential for the early detection and treatment of cellular alterations linked to HPV. These screenings include Pap tests and HPV testing. HPV vaccination dramatically lowers the chance of infection and cancer development later on, underscoring the need for preventative healthcare practices.
Previous History of Cervical Cancer: The likelihood of a woman having vaginal cancer is higher for women who have previously been diagnosed with the cervical cancer. This increased risk is a result of the possibility that cancerous cells would move from the cervix to the vaginal tissues, in addition to the fact that there are shared risk factors, such as an infection with the human papillomavirus (HPV). Furthermore, therapies for cervical cancer, such as radiation therapy, have the potential to make the vaginal tissues more susceptible to the development of malignant alterations. To discover any signs of vaginal cancer at an early stage, women who have a history of cervical cancer need to get regular follow-up care and diligent monitoring for any new symptoms that may appear without warning.
Age: There is a considerable correlation between age and the development of vaginal cancer, with the majority of cases emerging in women who are over the age of sixty. As women get older, their cells go through a process of change, and the cumulative exposure to various risk factors over their lifetimes results in an increased possibility of cellular abnormalities. In addition, as people age, their immune systems become less effective in repairing damaged DNA and controlling aberrant cell growth, all of which contribute to an increased likelihood of developing cancer.
The vaginal epithelium is more susceptible to carcinogenic impacts in postmenopausal women because of hormonal changes that alter the vaginal epithelium. This situation makes postmenopausal women particularly vulnerable. Having regular gynecological examinations becomes increasingly important as one gets older since these examinations can assist in the detection of early signs of vaginal cancer and other illnesses that are associated with aging. Older women should be encouraged to seek timely medical advice and tests if they know the increased risk associated with aging. It can help in the early detection of potential health problems and improve outcomes.
Radiotherapy on the Pelvis: Vaginal cancer risk may increase as a result of radiation treatment for pelvic cancers, such as endometrial or cervical cancer. The vaginal lining is among the healthy surrounding tissues that can sustain harm from the high-energy radiation used to eradicate cancer cells. This harm raises the possibility of malignant transformations and can result in long-term cellular alterations. After pelvic radiation therapy, healthcare providers should continuously monitor women for any signs of recurrent malignancies, such as vaginal cancer.
Higher dosage recipients and situations where the lower pelvis was within the radiation field are at greater risk. Routine follow-up treatment with a healthcare provider is necessary to identify any abnormal changes early on. Understanding this risk can help prevent and manage the long-term adverse effects of cancer therapy by encouraging preventive health practices like routine pelvic exams and quick investigations of any unexpected symptoms.
Smoking: Medical research has well-established tobacco as a risk factor for various malignancies, including vaginal cancer. The carcinogens that are included in tobacco smoke have the potential to damage the reproductive organs as well as the rest of the body. These potentially dangerous compounds have the potential to produce genetic abnormalities and damage the DNA of vaginal cells, which can ultimately result in aberrant cell development and cancer. Furthermore, smoking impairs the immune system, which in turn reduces the body’s ability to fight off infections such as HPV, which further raises the risk of developing vaginal cancer.
The duration and intensity of smoking are strongly associated with the risk, with those who have been smoking for a longer period being at a more significant risk. Kicking the habit of smoking can dramatically lower the likelihood of acquiring vaginal cancer as well as other types of cancer. Individuals can be motivated to adopt healthier lives and seek support for quitting smoking if they are aware of the link between smoking and vaginal cancer. This, in turn, can contribute to a better overall health and cancer prevention.
HIV Infection: HIV infection affects the immune system, which raises the risk of vaginal cancer. HIV increases a person’s vulnerability to cancer, especially HPV-related malignancies, by impairing the body’s defenses against infections and aberrant cell growth. HIV-positive women are more likely to get recurrent HPV infections, which can lead to precancerous lesions that eventually become vaginal cancer. For women living with HIV, routine gynecological exams and HPV tests are especially crucial to identify and treat any unusual changes as soon as possible. Antiretroviral therapy (ART) lowers the incidence of HPV-related malignancies while also assisting in immune system maintenance. Raising awareness and providing preventative care can improve outcomes for HIV-positive women, emphasizing the significance of routine check-ups and adherence to treatment plans.
Chronic Vulvar Itching or Irritation: There is some evidence that chronic vulvar itching or irritation may play a role in the development of vaginal cancer. Persistent irritation and inflammation can cause cellular changes, which in turn can increase the likelihood of malignant transformations occurring in the vaginal tissues. Several conditions can cause persistent discomfort and damage to the delicate vaginal lining. Some of these conditions include lichen sclerosis and chronic infections. Women who have persistent itching or irritation of the vulvar region should seek a medical examination to identify the underlying cause of the condition and obtain suitable treatment.
It is possible to lessen the likelihood of developing long-term problems, such as cancer, by effectively managing these disorders. Women can be encouraged to address their symptoms promptly if they are aware of the potential relationship between chronic vulvar disorders and vaginal cancer. It will ensure that they receive timely diagnosis and treatment, which will avoid the progression of the condition to cancer.
Alcohol: There is a correlation between drinking alcohol and an increased chance of developing several different malignancies, including vaginal cancer. Alcohol is metabolized, which results in the production of acetaldehyde, a poisonous chemical that can cause damage to DNA and proteins, which can ultimately lead to cellular alterations and the development of cancer. Additionally, alcohol can hurt the immune system, making it less responsive to the detection and repair of injured cells. Women who drink alcohol regularly and consistently consume significant amounts of it are in greater danger.
Consuming less alcohol can help lessen the risk of developing cancers of the vaginal and other types. Public health professionals can encourage healthier lifestyle choices and reduce the number of cancers caused by alcohol consumption by educating the general public about the risks of drinking alcohol and the link between it and cancer. Through the promotion of moderation and awareness, one can contribute to improved general health and cancer prevention.
Vaginal Adenosis: When glandular (columnar) cells, typically found in the cervix, are present in the vaginal lining, we call it vaginal adenosis. Diethylstilbestrol (DES), a synthetic estrogen that was provided to expectant mothers during the 1940s and 1970s to prevent miscarriages, is most commonly associated with this illness in women. Although vaginal adenosis is benign in and of itself, it can raise the risk of vaginal clear-cell adenocarcinoma.
Healthcare providers recommend regular gynecological exams for women previously exposed to DES to check for alterations in the vaginal tissue. Treating precancerous alterations as soon as they are identified can stop vaginal cancer in its tracks. Understanding the possible dangers associated with DES exposure is essential for efficient monitoring and timely management, which will eventually lower the risk of vaginal cancer in this high-risk population.
Family History of Vaginal Cancer: Genetic predispositions can raise an individual’s risk of vaginal cancer if there is a family history of the disease. Vaginal cancer is one of the inherited disorders and genetic alterations that might increase one’s risk of acquiring cancer. Women who have a family history of gynecological cancers, including vaginal cancer, should talk to their healthcare professional about their risk. Genetic testing and counseling can direct preventive steps and offer helpful information about individual risk. For those with a family history of cancer, proactive health monitoring and routine screenings are crucial for early identification. Understanding her genetic predispositions can enable women to take charge of their healthcare, resulting in prompt interventions and better overall outcomes for the management and prevention of vaginal cancer.
Prevention and Screening
Adopting multiple preventive measures is necessary to prevent vaginal cancer. Getting the HPV vaccine, which guards against high-risk strains of the human papillomavirus known to cause vaginal and other gynecological malignancies, is one of the most effective preventative measures. Frequent screenings—such as HPV and Pap tests—are crucial for the early identification of precancerous alterations, which enables prompt intervention and treatment.
Keeping the vagina healthy is also essential for prevention. It entails using safe sexual practices to lower the chance of STDs, abstaining from tobacco and alcohol, maintaining a nutritious diet to boost immune system function, and so forth. In addition, women should be alert to any strange symptoms and should consult a doctor right away if they have discomfort, abnormal vaginal bleeding, or discharge.
Regular medical check-ups, along with risk factor education and awareness, can greatly lower the incidence of vaginal cancer. Through the use of these preventive steps in their daily lives, women can take responsibility for their health and reduce their risk of vaginal cancer.
Treatment Options

Treatment for vaginal cancer depends on stage, type, and condition. Surgery, radiation therapy, chemotherapy, and the targeted therapy are the main treatments. Surgery usually removes the tumor and surrounding tissue. In advanced cases, however, surgeons may need to perform a radical hysterectomy. Radiotherapy kills cancer cells, either outside or internally. Chemotherapy kills or slows cancer cell proliferation as a standalone or combined treatment. Traditional chemotherapy is less precise than targeted therapy, which targets cancer cell growth and spread molecules.
Doctors must tailor treatment approaches to each patient’s cancer type, stage, and health. A diverse team optimizes efficacy and minimizes adverse effects to ensure the optimum outcome. Specialists must work together and monitor patients to adjust treatment and improve quality of life and recovery.
Conclusion
For efficient prevention and early detection, it is essential to comprehend the causes of vaginal cancer, which include HPV infection, age, radiation therapy, smoking, and hereditary factors. Make vaginal health a priority by getting vaccinated against HPV, going for routine screenings, and leading a healthy lifestyle can drastically lower the risk. As soon as you notice any strange symptoms, consult a doctor. The key to preventing vaginal cancer is to remain vigilant and knowledgeable. See your healthcare practitioner or trustworthy websites like the National Cancer Institute and the American Cancer Society for additional information and assistance.
In this Article

















