Affiliate Disclaimer
Some links in this article are affiliate links. We may earn a small commission if you make a purchase through these links, at no extra cost to you. We only recommend products we find useful to our readersDigestive health plays a fundamental role in how your body processes and absorbs nutrients, including glucose, the primary source of energy. The stomach, intestines, and associated organs break down food and ensure that nutrients are absorbed into the bloodstream, balancing blood sugar levels and maintaining metabolic health.
For individuals with diabetes, maintaining good gut health is not just about digestion; it’s crucial for optimal glucose absorption and regulation. Disruptions in gut health can directly impact blood glucose levels, making diabetes management difficult. Hence, improving gut health becomes crucial for diabetic patients.
The absorption of glucose is severely hampered when digestive health is compromised, causing a variety of conditions, such as gut dysbiosis and inflammation, leading to potential problems in glucose metabolism. Understanding how digestive health influences glucose absorption is crucial for managing blood sugar levels and preventing diabetes and metabolic syndrome.
In this article, we will talk about the intricate relationship between digestive health and glucose absorption. We will also analyze how gut microbiota, gut barrier function, and some common digestive disorders interfere with glucose metabolism. Further, we will discuss the diet and lifestyle factors that support digestive health and optimize glucose absorption.
By understanding this link between gut health and glucose absorption, you will understand how to promote healthy digestion, maintain stable blood sugar levels, and manage your diabetes.
Also, read: How Lifestyle Choices Affect Insulin Sensitivity
Digestive System Anatomy and Function
The digestive system is designed to take in food and convert it into energy and nutrients our body needs to function. At one end of this system is the mouth, and at the other is the anus, between which is a long series of organs working in perfect harmony, and here’s how this complicated system works:
Anatomy
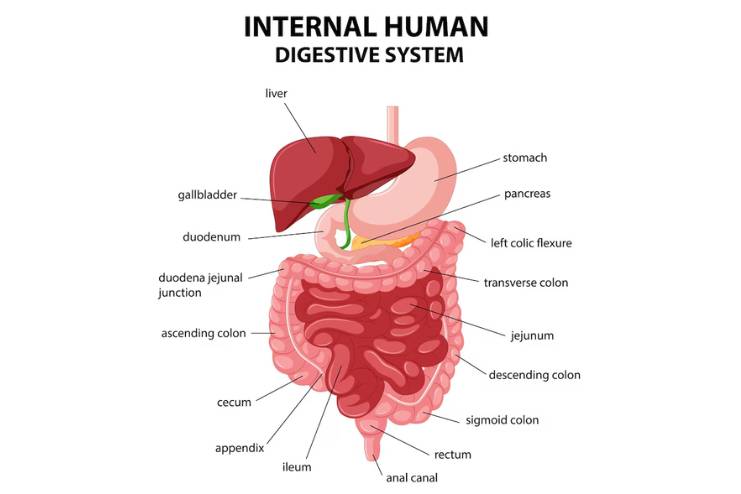
Gastrointestinal (GI) Tract
- Mouth: This is where it all starts. Carbohydrates start breaking down with the saliva. Mechanical food breaks down when you chew food into smaller food particles. The tongue thrusts it downwards towards the throat.
- Esophagus: This muscular tube carries food from the mouth into the stomach through peristalsis (repeated contractions). The lower esophageal sphincter regulates the food entering the stomach, preventing reflux.
- Stomach: This organ is completely hollow, and food mixes with gastric juices. These juices include strong acids and enzymes that further degrade proteins and prepare food for absorption. The stomach empties its contents into the small intestine in a semi-liquid substance known as chyme.
- Small Intestine: The intestines consist of three parts: the duodenum, jejunum, and ileum. The duodenum is a long tube that stretches 22 feet in length and is responsible for most digestion and nutrient absorption. Enzymes from the pancreas and bile from the liver help break down food. Nutrients are absorbed through the walls of the intestines into the bloodstream.
- Large Intestine (Colon): The large intestine absorbs water and electrolytes from the remaining undigested food matter and compacts it into the stool. It includes the cecum, ascending, transverse, descending, and sigmoid colon. The stool is kept inside the rectum until expelled from the body.
- Rectum: This reservoir chamber holds the stool until it is sufficiently ready to be expelled from the body. Sensors in the rectum signal the brain that a bowel movement is required.
- Anus: This is the final portion of the digestive tract, which maintains control over stool expulsion through the means of two sphincters, thus maintaining continence and placing voluntary control over bowel movements.
Also, read: How Insulin Resistance Impacts Your Heart Health
Biliary System
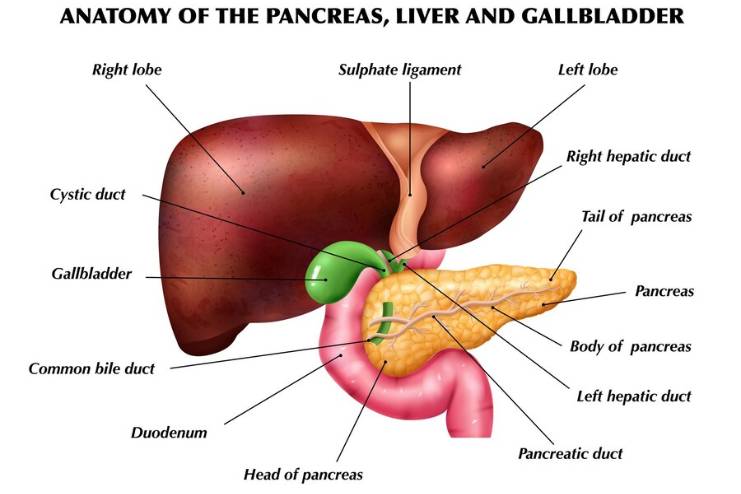
- Liver: It breaks down ingested nutrients absorbed in the small intestine, serves as a chyme producer to assist with the digestion of fats, and filters out harmful substances. This is the chemical factory that changes raw materials to essential chemicals and hormones.
- Gallbladder: It stores and thickens bile produced in the liver and releases it through the bile duct into the small intestine to assist in the breakdown of fats.
- Pancreas: It produces digestive enzymes that break down proteins, fats, and carbohydrates inside the small intestine. It also secretes insulin, which regulates blood sugar, directly into the bloodstream.
Function
The primary function of the digestive system is to break down food we eat into nutrients and energy. It breaks down food into tiny molecules so the body can absorb it, while waste products are eliminated from the body through bowel movements. A healthy digestive system ensures all essential nutrients are absorbed and waste removed efficiently.
Understanding the anatomy and physiology of the digestive system is critical for recognizing how it impacts overall health and participates in glucose absorption. Any disruptions in this system trigger inefficient nutrient processing and metabolic imbalances, including issues with glucose regulation.
Also, read: 12 Best Glucose Meter For Keeping Your Sugar Levels In Control
Impact of Gut Health on Glucose Absorption
Gut health plays a crucial role in glucose absorption; hence, balancing blood sugars is essential. Carbohydrates must be broken down by the gut or the gastrointestinal (GI) tract, turning them into glucose, which is then absorbed into the bloodstream. Several factors associated with gut health impact this function, influencing glucose metabolism and general metabolic health. Here’s how:
1. Gut Microbiota and Glucose Metabolism
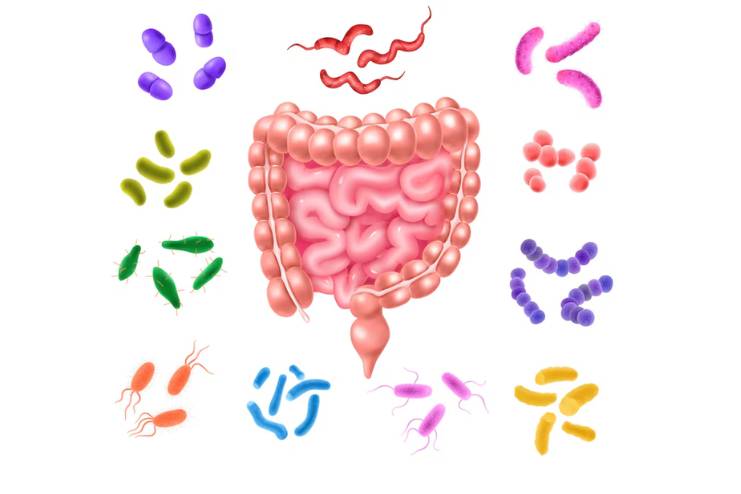
The gut microbiota, the community of microorganisms that reside in the intestines, greatly influences glucose metabolism. A balanced and diverse microbiota supports digestion and nutrient absorption. Microorganisms such as Bifidobacteria and Lactobacillus, for example, are known to enhance fiber fermentation and produce SCFAs, including acetate, propionate, and butyrate, which contribute to the integrity of the gut lining and may serve to modulate glucose metabolism:
- Enhancing Insulin Sensitivity: SCFAs enhance cell sensitivity to insulin, allowing cells to better utilize glucose and, hence, lower blood glucose levels.
- Regulating Appetite: SCFAs stimulate the release of hormones responsible for hunger and satiety, which could indirectly affect caloric intake and blood glucose.
- Modulating Inflammation: A good microbiota is believed to suppress systemic inflammation. Increased systemic inflammation is associated with insulin resistance and poor glucose homeostasis.
2. Intestinal Barrier Function
For glucose to be absorbed properly, the gut barrier must be integrated well. A healthy gut lining prevents the entry of toxins and disease-causing pathogens into the blood circulation. Disruptions to the gut lining, such as those caused by leaky gut syndrome, expose a person to:
- Increased Inflammation: Endotoxins pass into the bloodstream, triggering an inflammatory response after bypassing the compromised barrier. Inflammation may interfere with insulin function and lead to even higher sugar levels in the blood.
- Altered Nutrient Absorption: The compromised mucosa will impair nutrient absorption, including glucose, that regulates blood sugar variability.
3. Digestive Enzyme Activity
Digestive enzymes are vital to break down carbohydrates into glucose. Enzymes produced by the pancreas include amylase, which initiates the process of breaking down starches at the mouth and continues working in the small intestine. Optimal enzyme functioning ensures efficient breakdown and absorption of glucose. Conditions affecting enzyme production or activity, such as pancreatic insufficiency, may cause:
- Inadequate Glucose Absorption: Low activity of digestive enzymes results in poor carbohydrate digestion. Hence, starch remains undigested for the gut bacterium to ferment in the large intestine, sometimes causing bloating and gas.
- Uncontrolled Blood Sugar Levels: Poor absorption of glucose may result in blood glucose spikes and generally affect glucose control.
4. Fiber Intake and Gut Health

Dietary fiber, particularly soluble fiber, plays a significant role in glucose absorption. Soluble fiber slows the absorption of glucose, leading to:
Dietary fiber, particularly soluble fiber, plays a key role in glucose absorption. Soluble fiber slows glucose absorption, leading to:
- Gradual Blood Sugar Rise: Fiber slows digestion and therefore not result in a rapid increase in blood glucose levels after food intake.
- Improved Glycemic Control: A diet high in fiber, including fruits, vegetables, and whole grains, may improve glycemic control to help maintain metabolic health.
Also read: Tips to Reduce Too Much Fiber in Your Diet
5. Influence of Probiotics
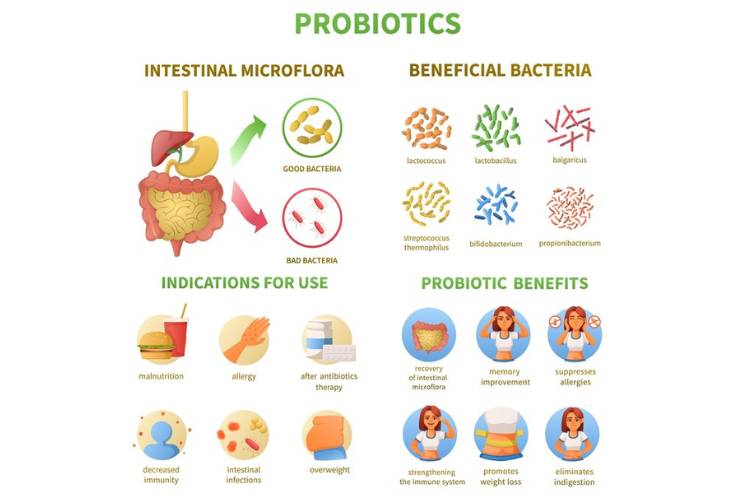
Beneficial bacteria, or probiotics, can influence the gut positively and help in glucose metabolism. Supplementing with probiotics through food, by including yogurt and fermented vegetables, may:
- Improve Insulin Sensitivity: Probiotics enhance insulin sensitivity, balancing blood glucose.
- Reduce Inflammation: The anti-inflammatory properties of probiotics can help improve gut barrier function, further supporting healthy glucose metabolism.
6. Impact of Stress and Lifestyle Factors

Stress and other lifestyle factors affect gut health and glucose absorption. Chronic stress changes a person’s balance of gut microbiota and impairs barrier function in the gut, leading to:
- Increased Blood Sugar Levels: Stress hormones, which include cortisol, increase blood sugar levels and contribute to insulin resistance.
- Altered Digestive Function: Stress can decrease the production of digestive enzymes and disrupt gut motility, impacting normal glucose absorption and overall metabolic health.
Also, read: 20 Stress Relieving Foods Help You Reduce It Instantly- Must Know!
Conclusion
Digestive health affects the breakdown of carbohydrates and their absorption into the bloodstream. Therefore, digestive health entails regulating glucose absorption into the bloodstream, which has an overall impact on metabolic function and the control of blood sugars.
A disturbed balance in the gut microbiota, disrupted intestinal barrier function, low enzymatic activity, or a diet with insufficient fiber can lead to an impairment in potential metabolic disorders. A balanced gut microbiota, an effective intestinal barrier, optimal enzyme functioning, and a fiber-rich diet are required for efficient glucose absorption. However, probiotics and stress management can also help with healthy digestion and stable blood sugar levels.
By understanding these connections and prioritizing digestive health, you can better manage your glucose levels and reduce the risk of metabolic disorders.
For diabetic patients, focusing on gut health is key to managing blood sugar levels. A healthier gut can improve glucose absorption and insulin sensitivity, reducing the risk of complications associated with diabetes. By supporting digestive health, patients can take a proactive step in their overall diabetes care plan.
Promote healthy digestion through a balanced diet, regular exercise, and effective stress management. These factors enhance glucose absorption and overall well-being. Continued investigation into this complex relationship between gut health and glucose metabolism will further provide more targeted strategies for blood sugar management and metabolic health.
References
- https://my.clevelandclinic.org/health/body/7041-digestive-system
- https://my.clevelandclinic.org/health/treatments/14598-probiotics
- https://indisupplements.com/blogs/nutrition/the-impact-of-gut-health-on-blood-sugar-levels
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6104804
- https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/fiber/art-20043983
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7213601
In this Article