Affiliate Disclaimer
Some links in this article are affiliate links. We may earn a small commission if you make a purchase through these links, at no extra cost to you. We only recommend products we find useful to our readersDiabetic patients are more prone to developing serious eye conditions, which may result in vision loss or even complete blindness if untreated. As with most diabetic complications, the only way to detect and treat these early, before noticeable symptoms appear, is through eye exams. Routine eye checkups can prevent these complications and maintain healthy vision.
Common Diabetic Eye Conditions

Diabetes, over time, can cause many severe eye issues. High blood sugar levels damage the lenses and blood vessels in the eyes. Complications with diabetes not only affect the vision but can also cause complete blindness if they are not treated in time.
Some of the most common diabetic eye problems are:
1. Diabetic Retinopathy
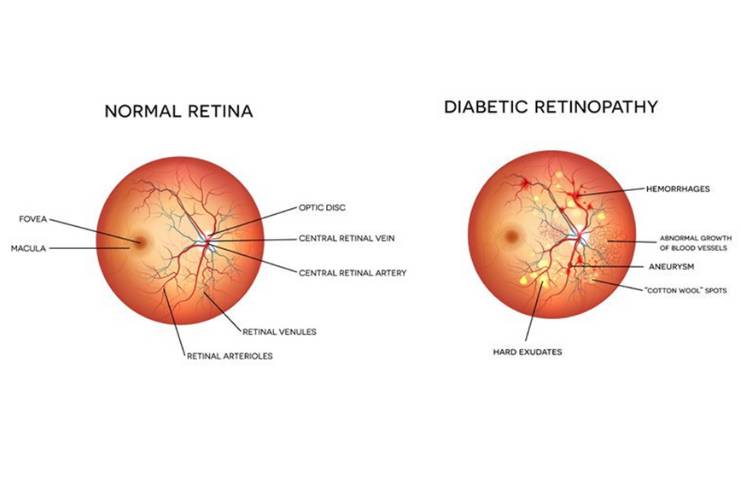
In the United States, diabetic retinopathy is the leading cause of blindness in adults. This is because high blood sugar levels affect the blood vessels in the retina, the tissue at the back of your eye that’s sensitive to light. Sometimes, these vessels may swell, leak fluid, or bleed, which can lead to vision loss. Untreated diabetic retinopathy can create retinal detachment, a condition in which the back of the eye will pull away and cause permanent blindness.
2. Diabetic Macular Edema (DME)
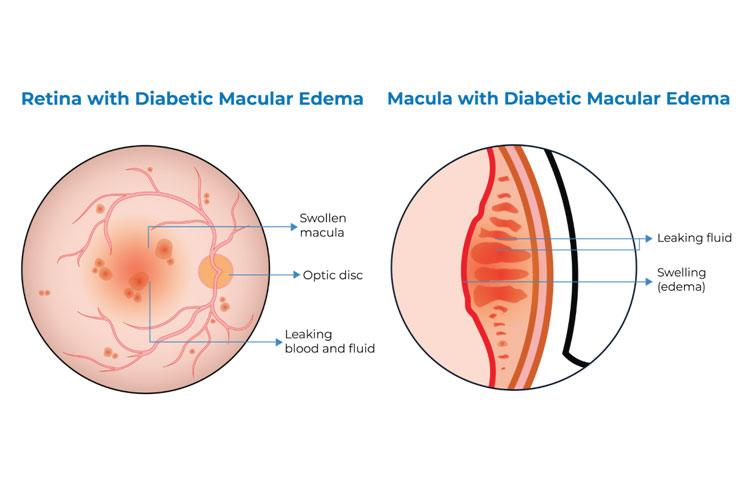
DME develops as a complication of diabetic retinopathy and is caused by the leakage of fluid from damaged blood vessels into the macula, a part of the retina that is responsible for sharp central vision. It causes blurring or distortion of vision, which in turn, due to its adverse effects on daily life, should be treated immediately.
3. Glaucoma
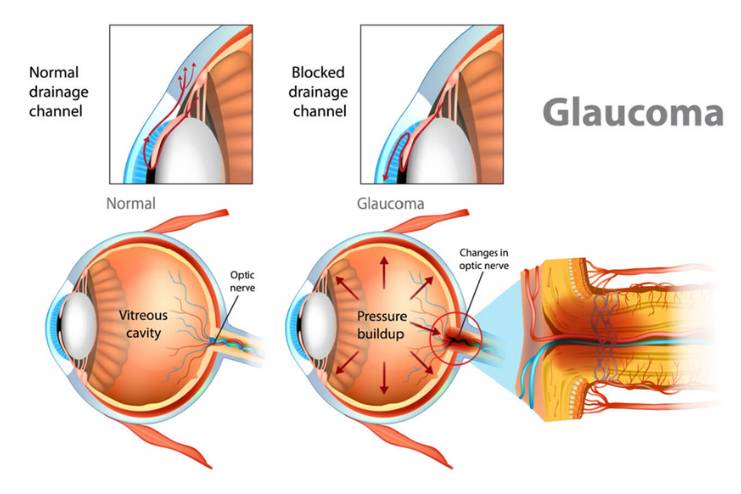
Diabetes increases the risk for glaucoma. It is a group of eye diseases that damage the optic nerve responsible for transmitting visual information to the brain. Damage causes blockage of fluid drainage near the iris, the colored part of the eye, which results in increased eye pressure, damages the optic nerve and eventually leads to loss of vision if not treated in time.
4. Cataracts
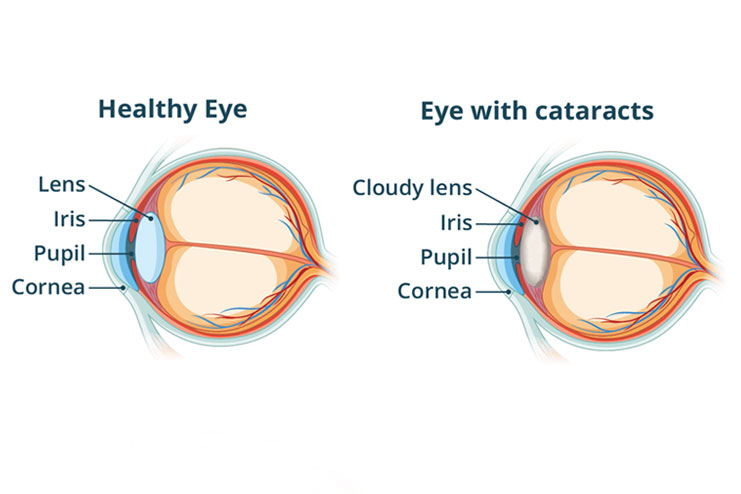
Cataracts occur when the clear lens of the eye becomes cloudy, making it difficult to see clearly. While cataracts are common with aging, individuals with diabetes are at higher risk of developing them earlier and progressing more rapidly. High blood sugar may contribute to the buildup of deposits in the eye’s lens, accelerating cataract formation and impairing vision.
You may also want to understand the impact of high blood sugar on vision
What Increases the Risk of Developing Diabetic Eye Conditions?

- Duration of Diabetes: The longer an individual has diabetes, the more susceptible they become to developing diabetic eye complications. This includes diabetic retinopathy, macular edema, and even glaucoma. Victims who have had diabetes for 10 to 15 years are at a very high risk.
- Poor Blood Sugar Control: People struggling to keep their blood glucose levels within the normal range are more prone to damage to the blood vessels in the eye. Diabetic eye diseases come directly from this damage. Consistently high glucose levels in the eyes accelerate the development of complications.
- High Blood Pressure and Cholesterol: High blood pressure and cholesterol continue damaging the blood vessels in the retina, increasing the risk of diabetic retinopathy and other eye diseases. Hence, proper management of these factors can keep these problems at bay for preserving eyes.
- Pregnancy: Pregnant women with diabetes have a higher risk of developing diabetic retinopathy, especially if the diabetic eye problem preexists even before pregnancy. Regular follow-up and proper control of blood sugar during pregnancy are vital to reduce such a risk.
- Smoking: Smoking exacerbates diabetes-associated conditions and makes an individual vulnerable to complications in the eye. This leads to the obstruction of blood flow in the retina and accelerates the deterioration of blood vessels.
- Genetics: Genetic factors are also known to contribute to the complications of diabetic eye diseases. A person with a family history of diabetic retinopathy or any other condition associated with it is more likely to suffer from these complications.
Why Regular Eye Exams are Crucial

With early detection, complications can be minimized through proper treatment. You can book appointments with an optometrist or an ophthalmologist for regular eye check-ups as part of a scheduled consultation.
- Identify early signs of diabetic eye diseases: Through regular eye exams, doctors are able to detect these microscopic changes in the retina, including microaneurysms or retinal hemorrhage, that can serve as indicators of an early onset of diabetic retinopathy. These often occur well before symptoms appear.
- Monitor the progression of diabetic eye diseases: Regular exams help track any progression of existing eye problems. For example, diabetic retinopathy worsens with time if not treated.
- Prevent vision loss: Early intervention through laser treatment, medications, or other forms of therapy can prevent or slow the vision loss that diabetic eye diseases commonly cause.
- Identify and address potential complications: Diabetes eye exams also identify other eye conditions like cataracts and glaucoma, which may be worsened by diabetes.
Components of a Diabetic Eye Exam

An eye exam for diabetics typically includes:
- Visual Acuity Test: This is the test that determines how clearly you can see from a distance when you read letters or numbers on a chart from a specified distance to find out if you have a condition that requires corrective lenses.
- Pupil Dilation: Your doctor will use eye drops to dilate your pupils. This procedure momentarily enlarges your pupils so that the doctor can have a better view of your retina and check for diabetic retinopathy and other issues in the back of your eyes.
- Retinal Examination: Your doctor will check your eyes with an ophthalmoscope or other equipment for signs of diabetic retinopathy, such as microaneurysms, tiny bulges in blood vessels, retinal hemorrhages (bleeding), or cotton wool spots (areas of nerve fiber damage). These signs represent the damage caused in your bloodstream.
- Glaucoma Testing: In this test, pressure inside the eyes is tested. High pressure may indicate glaucoma, a condition that can damage the optic nerve by sacrificing vision.
- Color Vision Test: Diabetic retinopathy patients often experience a change in color vision, and this test helps to identify early signs of the disease.
Regular exams are hence critical for early detection to prevent and manage diabetic eye diseases.
How a Diabetic Eye Exam Differs from a Standard Eye Exam

While diabetic eye exams share many similarities with regular eye exams, they focus more on the condition of the retina and the state of blood vessels in the eyes.
Apart from that, one main difference is the pupil dilation administration, which is part of the regular diabetic eye exam procedures. With dilation of the pupils, the eye doctor can see a live view of the retina, optic nerve, and blood vessels, thus spotting early diabetic retinopathy and its complications.
Special eye drops are used to dilate the pupils, and it takes some time, usually about half an hour, before these drops start acting. Dilation causes blurring in the near vision, which could last for a few hours, and sensitivity to light. However, this is essential for detecting many abnormalities that may not easily be seen during the non-dilated eye examination.
In some cases, additional tests may be recommended following the retinal examination. These can include retinal imaging, fluorescein angiography (a test that highlights blood flow in the retina), or optical coherence tomography (OCT), which provides detailed cross-sectional images of the retina. These advanced diagnostic tools help in the early detection and management of diabetic eye diseases.
These tests may include the following:
- Retinal imaging
- Fluorescein angiography
- Optical coherence tomography (OCT)
This specialized approach in diabetic eye exams makes it possible to determine and treat an early condition, which can severely impact vision if the condition goes untreated.
How Often Should Diabetics Have Eye Exams?

The frequency of eye tests depends on the type of diabetes and the severity of the existing complications in the eyes.
- Type 1 Diabetes: Patients with type 1 diabetes should undergo a full eye checkup within five years after its onset because this type of diabetes starts at a very young age. After that, it is recommended to opt for annual eye checkups to detect any emerging problems.
- Type 2 Diabetes: Type 2 diabetics should also get an eye exam shortly after diagnosis, as the disease may have been present for a long time before diagnosis, increasing the chances of eye problems. A yearly exam is recommended thereafter, just like type 1 diabetes.
- Pregnant Women with Diabetes: For pregnant women, the risk of diabetic retinopathy increases. Therefore, women with diabetes who intend to get pregnant or are pregnant should have a comprehensive eye exam in their early pregnancy phase. Follow-up exams may be recommended throughout pregnancy according to their eye condition.
- High-Risk Individuals: People with more advanced diabetic retinopathy or a more severe eye disease should do frequent follow-ups, such as every 6 months, to monitor their condition and adjust treatment as necessary.
The Risks of Skipping Regular Eye Exams for Diabetes

Failure to schedule regular eye exams may result in serious and often permanent consequences for people with diabetes. Diabetic eye diseases tend to develop without any symptoms, causing almost no pain and showing signs only when the damage is already done.
The following are the significant risks of skipping eye checks:
- Undiagnosed Diabetic Retinopathy
- Worsening of Diabetic Macular Edema (DME)
- Increased Risk of Glaucoma and Cataracts
- Missed Opportunities for Preventive Care
- Permanent Vision Loss
Conclusion
Regular eye exams form an important component of diabetes care, a crucial preventive measure against severe complications caused by this condition. The risk of serious eye problems such as diabetic retinopathy, macular edema, glaucoma, and cataracts increases with diabetes, making early detection and intervention crucial in maintaining vision and quality of life.
Prioritizing regular eye checkups thus would enable a diabetic to take necessary proactive measures toward eye health. Apart from the benefit of early detection, diabetics can continue their normal daily lives without constantly worrying about their vision.Diabetes
References
- https://medlineplus.gov/diabeticeyeproblems.html
- https://maduraieyecenter.com/regular-eye-exam-for-diabetic-patients
- https://medlineplus.gov/ency/patientinstructions/000323.htm
- https://www.optos.com/blog/2023/november/Diabetic-Eye-Exams/
- https://www.ncbi.nlm.nih.gov/books/NBK582424/
- https://www.medicalnewstoday.com/articles/diabetic-eye-exam
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6389265/
In this Article