Affiliate Disclaimer
Some links in this article are affiliate links. We may earn a small commission if you make a purchase through these links, at no extra cost to you. We only recommend products we find useful to our readersThe insulin, secreted by the pancreas, is a critical hormone that significantly controls glucose levels in the blood by allowing cells to uptake glucose for energy. In the case of type 1 diabetes, the patient’s immune cells mistakenly attack the beta cells in the pancreas, which produce insulin; consequently, the body becomes insulin-deficient.
Thus, patients with type 1 diabetes have no choice but to control their blood sugar by insulin treatment. In this article, we will discuss insulin production, its function in glucose metabolism, and insulin therapy’s role in the effective management of type 1 diabetes.
Insulin Production in the Pancreas
Insulin is a hormone that plays a critical function in controlling blood sugar. It was the first hormone discovered, but it later became a protein.
Insulin comprises two chains, the A-chain and B-chain, linked together by unique disulfide bonds. Before it becomes active, insulin exists in a larger inactive form called proinsulin.
Steps of Insulin Production:
- Preproinsulin Formation: The process begins with developing a preproinsulin molecule. This molecule has a “signal peptide” that helps guide it into a part of the cell known as the endoplasmic reticulum (ER). The signal peptide cleaves off in the ER, and proinsulin remains.
- Proinsulin Folding and Bonding: Once in the ER, the proinsulin molecule folds and forms disulfide bonds. Folding is very important since it enables insulin to assume its proper shape. However, proinsulin is still not an active hormone that the body needs at this stage.
- Conversion to Insulin:
The proinsulin is then carried to the Golgi apparatus, the cell’s portion that packages it into small storage units called secretory granules.
In secretory granules, the proinsulin is broken apart into insulin and C-peptide. Enzymes that cleave the proinsulin molecule at specific points remove a section referred to as the C domain.
The output is mature insulin that can be released into the blood. Along with the insulin, another molecule known as C-peptide is secreted, which does not affect blood glucose levels.
- Release of Insulin: Insulin release into the bloodstream leads to a drop in blood sugar concentration because the glucose is utilized by body cells. This happens during food consumption when the blood glucose concentration increases. Cells then take glucose from the blood through the secreted insulin molecules in the body.
Role of Enzymes in Insulin Production
Some specialized enzymes cut proinsulin to liberate insulin. These two enzymes, prohormone convertases PC1/3 and PC2, work together to remove the C-peptide and give the insulin molecule the finishing touches.
Another enzyme, carboxypeptidase E, cleans up the remaining residues so that insulin should be fully active.
Insulin Storage and Release
After synthesis, insulin is packaged in granules within the pancreas’s beta cells. These granules release insulin into the blood circulation in response to high blood glucose concentration.
Therefore, as long as the body functions normally, insulin production and release are precisely regulated according to changes in blood glucose concentration.
Role of Insulin in Glucose Metabolism
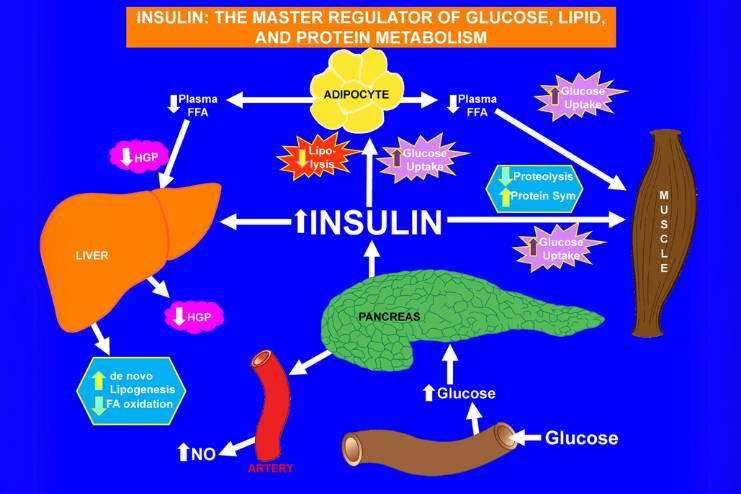
How Insulin Works in Glucose Metabolism
As soon as you eat your meal, your pancreas secretes insulin because the glucose in your bloodstream rises. Once the insulin attaches to its receptor on the cell membrane, it behaves like a “key” that opens up the cell to let glucose enter it to be used for fuel.
If you do not have enough insulin, glucose accumulates in the blood because it cannot enter the cell.
When too much glucose is in the bloodstream, insulin directs the body to reserve glucose in the liver, muscles, and fat cells.
The stored glycogen can then be broken down back into glucose and utilized to sustain energy when time lapses between meals or when the body is physically active.
Insulin’s Role in Glycogen and Fat Storage
Insulin ensures that the excessive glucose is transformed into glycogen in the liver. However, if glycogen is stored maximally in the liver, then the excess glucose gets absorbed in the fat cells, and that is converted into fats, including lipoproteins.
Consequences of Insufficient Insulin
Without insulin, the body cannot utilize glucose, resulting in diabetes mellitus, which causes chronic hyperglycemia. Prolonged hyperglycemia eventually causes severe damage to the nerves, kidneys, eyes, and extremities.
During severe cases, when insulin is absent, the body utilizes fats as energy. This process releases ketones, which, if present in the body in quantities above normal, can cause ketoacidosis, a dangerous condition for life.
Additional Functions of Insulin
Apart from regulating blood sugar, insulin is involved in several other body functions:
- Modifying enzyme activity to control various body reactions.
- Helping build muscle after injury by transporting amino acids to repair and strengthen muscle tissue.
- Regulating fat storage by helping convert glucose into triglycerides in fat cells.
- Managing the breakdown of proteins and lipids in fat cells.
- Supporting the uptake of amino acids and potassium into cells.
- Regulating the excretion of sodium and fluid through urine.
- Enhancing brain functions like memory and learning.
Insulin Therapy in Type 1 Diabetes

People with type 1 diabetes need to take insulin for the rest of their lives because their bodies cannot produce it. Insulin therapy helps control blood sugar levels and mimics how the body naturally uses insulin.
Types of Insulin
There are several types of insulin, which have different timings of action and duration of action:
Immediate- or Short-Acting Insulin:
- It is absorbed into the body within about half an hour after injection.
- Onset peaks at 90 to 120 minutes and lasts 4 to 6 hours.
- Examples: Humulin R, Novolin R, Afrezza.
Rapid-Acting Insulin:
- Works in 15 minutes
- It rises at 60 minutes and lasts for about four hours.
- This insulin is most commonly used immediately before meals to control an elevation in blood sugar levels.
- Examples: Glulisine (Apidra), Lispro (Humalog, Admelog), and Aspart (Novolog, FiAsp).
Intermediate-Acting Insulin
- Works within 1 to 3 hours
- Rises at 6 to 8 hours and lasts 12 to 24 hours.
- Example: NPH insulin Novolin N, Humulin N.
- Intermediate and Long-Acting Insulin: Insulin coverage is provided for 14 to 40 hours, depending on the preparation.
Combination of Types of Insulin
To give the body an approximation of natural insulin output, most patients with type 1 diabetes require daily multiple injections. The most common regimen is injecting long-acting insulin for basic coverage, which will be stable all day.
Then, before each meal, rapid-acting insulin can be introduced to absorb the spikes in blood sugar levels produced by food intake. This is a much more effective method of controlling blood sugar levels compared to previous regimens that required just one or two shots a day.
Three or more daily injections have been found to improve blood glucose levels and decrease complications.
Challenges in Insulin Management

Type 1 diabetics have several challenges when it comes to maintaining appropriate levels of insulin. People on intensive regimens are perhaps most seriously challenged since this regimen is designed to reproduce as closely as possible the way a normal pancreas functions.
This usually keeps one’s blood sugar level as close to normal as possible. However, this kind of treatment has many problems.
Frequent Monitoring
Intensive insulin therapy requires multiple blood sugar checks, which may be needed four or more times daily or used in conjunction with a continuous glucose monitor (CGM).
This can be demanding and time-consuming because it requires coordination with daily activities such as eating, exercising, and working.
Hypoglycemia (Low Blood Sugar)
One of the critical risks with insulin therapy is hypoglycemia, or blood sugar that is too low. It can be caused when excess insulin is administered, meals are postponed, or physical activity occurs when not expected.
Thus, it is important to teach people how to prevent, recognize, and treat hypoglycemia so that they can be prepared to prevent complications from the condition.
Weight Gain
This can cause weight gain, especially when starting insulin therapy with intensive regimens. However, exercise regularly helps to minimize or even inhibit weight gain.
Costs
Intensive insulin therapy can be more expensive than more straightforward treatments. It often involves multiple daily insulin injections or the use of an insulin pump, and frequent blood sugar tests. While many insurance plans cover some of these costs, they can still add up for some patients.
Staying Motivated
The commitment required for intensive insulin management can be overwhelming. Due to the daily demands, some people may lose motivation over time.
Support from a healthcare team, along with resources from organizations like the American Diabetes Association (ADA) and the Juvenile Diabetes Research Foundation (JDRF), can help individuals stay on track.
Advances in Insulin Therapy

Recent advances in insulin therapy focus on improving glucose control and reducing side effects like hypoglycemia. Two ultra-long-acting basal insulins have emerged as significant innovations:
- Insulin Glargine U-300: It received FDA approval in 2015. It lasts longer than the older U-100 formulation, lowering the risk of nocturnal hypoglycemia. Clinical studies have shown that the U-300 is equivalent to the ubiquitous U-100 version in managing blood glucose levels (R).
The incidence of nocturnal hypoglycemia was found to be decreased in subjects receiving U-300. However, you would likely require a tad more insulin with U-300.
- Insulin Degludec (Novo Nordisk): Another is Insulin Degludec (R) by Novo Nordisk, approved in 2015. It lasts for at least 42 hours and causes less day-to-day variation in its effect compared to U-100 insulin.
Studies demonstrated it caused fewer low blood sugar episodes, especially at night, but it controlled blood sugar like other insulins (R).
These insulins provide better blood sugar control and fewer low blood sugar episodes, especially at night.
Other Innovations:
- Insulin 287: A once-weekly insulin Novo Nordisk is in the works to reduce the injection count.
- Oral Insulin: Pills like ORMD-0801 (R) are being tested to avoid injections and are unavailable yet.
- Inhaled Insulin: Afrezza (R) is a rapid-acting inhalable insulin approved in 2014. It is most effectively used as an adjunct to other insulins.
Ultra-Fast-Acting Insulins:
- Fiasp (Novo Nordisk): This insulin works faster than standard insulin due to added ingredients that speed up absorption. It also controls blood sugar after meals better than regular insulin.
- LY900014 (URLi): An ultra-fast insulin by Eli Lilly (R), still in testing, shows quicker blood sugar control after meals with fewer risks of low blood sugar.
These new insulins offer better blood sugar control with fewer side effects, making life easier for people who need insulin.
Conclusion
Advances in insulin therapy are represented by long-acting insulins like Insulin Glargine U-300 and Insulin Degludec, as well as other novelties such as ultra-fast-acting insulins and inhaled insulin.
These new-generation insulins control blood glucose levels better with fewer side effects, making managing diabetes more straightforward and effective. The risk of complications, predominantly hypoglycemia, especially at night, could be diminished.
Ongoing research into weekly insulin injections and oral insulin pills holds even more promise for the future of diabetes care.
References
In this Article

















