Affiliate Disclaimer
Some links in this article are affiliate links. We may earn a small commission if you make a purchase through these links, at no extra cost to you. We only recommend products we find useful to our readersThe two main types of inflammatory bowel disease (IBD), Crohn’s disease and ulcerative colitis, are more than just medical terminology; they are the everyday struggles of millions of people worldwide. These illnesses can cause significant disruptions to people’s lives by presenting a complicated web of erratic symptoms, such as persistent pain, exhaustion, and digestive issues.
Beyond the physical difficulties, however, there is an important reality: empowerment begins with understanding. In this article, we’ll cover the fundamentals of Crohn’s and colitis, their symptoms, and practical support advice. In addition to educating communities about the realities of living with IBD, this Crohn’s and Colitis Awareness Week acts as a catalyst for group action.
What is Crohn’s Disease and Ulcerative Colitis?
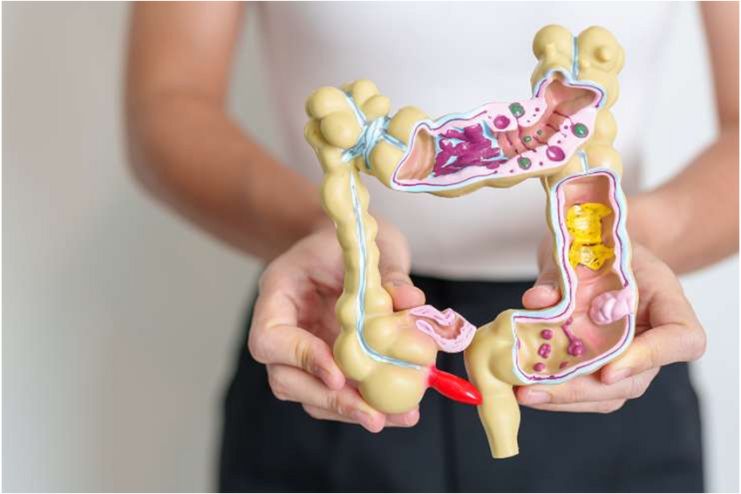
The two primary forms of inflammatory bowel disease (IBD), which are long-term illnesses that result in inflammation of the digestive tract, are Crohn’s disease and ulcerative colitis. Despite similarities, they pose distinct difficulties and impact different digestive system areas.
Crohn’s disease often affects the small intestine, but it can affect any region of the digestive system, from the mouth to the anus. It frequently affects the intestinal wall’s inner layers, resulting in weariness, weight loss, malnourishment, diarrhea (sometimes bloody), and abdominal pain.
Ulcerative colitis, in contrast, only affects the colon (large intestine) and rectum. It affects the colon’s interior lining, resulting in symptoms like urgent diarrhea, frequent bowel movements, rectal bleeding, and discomfort in the abdomen.
Although the precise causes of these disorders are unknown, experts believe that a mix of environmental factors, an overactive immune response, and genetic predisposition are responsible.
These illnesses can significantly impact your life, necessitating constant medical attention, dietary modifications, and lifestyle adaptations. By being aware of these disorders, we may promote proactive measures for support and treatment and empathy for individuals impacted.
Symptoms and Diagnosis

The complicated range of symptoms associated with Crohn’s disease and ulcerative colitis can differ from person to person and often interfere with day-to-day functioning in ways that only those impacted can fully comprehend.
Typical symptoms include prolonged diarrhea, intense stomach discomfort, appetite loss, unintentional weight loss, exhaustion, fever, elevated body temperature, and occasional anemia (low blood cell count). Since these symptoms fluctuate for many people, it can be difficult to predict when a flare-up will occur.
Doctors examine your medical and family history, conduct a physical examination, and prescribe tests to diagnose Crohn’s disease. Physicians prescribe tests like:
Family History and Health
- Your doctor will inquire about your symptoms
- Medical history
- Current medications
- Lifestyle choices like smoking.
Physical Examination
- A doctor typically looks for abdominal fat or bloating during a physical examination.
- Uses a stethoscope to listen for sounds coming from inside the abdomen.
- Applies pressure to your abdomen to check for lumps or sensitive spots.
- Examine your entire body to rule out other possible causes of your symptoms and look for signs of weight loss and inflammation in other areas.
Treatment Options
Numerous treatment options are available for Crohn’s disease and ulcerative colitis, customized for each patient’s particular path. Keep in mind that no single treatment will be effective for every patient. Every patient has a unique predicament requiring a specific course of action.
Medication, clinical trials, dietary and nutritional changes, and occasionally surgery to remove or repair damaged GI tract segments are all options for treating Crohn’s disease and other types of IBD.
Drugs:
Crohn’s disease medication aims to reduce the abnormal inflammatory response in your immune system that is causing your symptoms. In addition to relieving common symptoms, including fever, diarrhea, and pain, reducing inflammation promotes the healing of intestinal structures. Medication can reduce the frequency of the symptom flare-ups (maintaining remission) and control the suppressed symptoms (inducing remission).
Adalimumab is a medication for Crohn’s disease and colitis. Those currently using or considering this medication should read more about it in the link.
Crohn’s disease or colitis patients currently taking mercaptopurine or azathioprine, as well as those considering starting these medications. For more details, refer to this link to make an informed and personalized decision.
This information is for individuals with ulcerative colitis who are using etrasimod, also known as Velsipity, or considering starting therapy with this medication. Refer to this link to help decide if this treatment is right for you.
Nutrition & Diet:
Even though adverse food reactions cannot cause Crohn’s disease, a customized diet can help heal, replace lost nutrients, and reduce symptoms. Maintaining a healthy diet is crucial for those with Crohn’s disease because the condition frequently decreases appetite while raising energy requirements.
A diet rich in fruits and vegetables, low in omega-6 fatty acids, and high in omega-3 fatty acids may reduce your risk of Crohn’s disease or colitis. Nuts, seeds, leafy green vegetables, and oily fish are among the foods that contain omega-3 fatty acids.
Check out this helpful link for more information on how nutrition can play a crucial role in managing Crohn’s disease and ulcerative colitis.
Surgery:
Up to two-thirds to three-quarters of individuals with Crohn’s disease will need surgery at some time in their lives, even with proper medication and nutrition. Surgery can save parts of your GI tract and restore your quality of life.
Clinical Trials:
Clinical trials may offer a valuable option for individuals who are not responding to standard treatments for their IBD. These trials represent one of the final stages of a thorough and extensive research process, where new therapies and strategies are tested to improve patient outcomes. By participating in a clinical trial, individuals can access cutting-edge treatments while contributing to research that may benefit others in the future.
Lifestyle Tips for Managing Crohn’s and Colitis
Managing Crohn’s disease or ulcerative colitis necessitates striking a balance between mental and physical well-being. Modest but deliberate lifestyle adjustments can significantly impact symptom management and general well-being.
Dr. Eric Ibegbu, MD, and his team at Atlantic Medical Group emphasize the importance of comprehensive care for individuals with Crohn’s disease. Their approach highlights the value of incorporating lifestyle changes alongside medical or surgical interventions as part of a holistic treatment plan. Patients can achieve improved symptom control and overall well-being by:
- Whether you have Crohn’s disease or not, exercise is unquestionably beneficial for everyone. However, by lowering stress, exercise can help you live a better life if you suffer from irritable bowel illness. Stress is a significant cause of gastrointestinal distress, and research indicates that regular exercise helps manage stress and prevent flare-ups of Crohn’s disease.
- If you smoke, this is an excellent time to think about quitting. Smoking affects every aspect of your body, including your gastrointestinal tract, despite its well-known effects on the lungs. According to studies, smoking raises your chance of getting Crohn’s disease and can exacerbate it in people who already have it.
- Stress levels and your stomach are related. Anyone can experience an upset stomach while under a lot of stress, but stress can trigger a flare-up in people with Crohn’s disease if not controlled. Exercise, yoga, meditation, journaling, listening to relaxing music, and talk therapy are some methods for managing stress.
Supporting a Loved One with Crohn’s or Colitis

Providing emotional and practical support might be crucial for a loved one coping with Crohn’s disease or ulcerative colitis. It’s critical to create a sympathetic and understanding atmosphere that recognizes the unseen challenges of having IBD.
- It should come as no surprise that IBD affects people emotionally, leading to anxiety and sadness in many cases.
- Being adaptable is the first step in creating a supportive home environment. Always understand when your loved one needs to rest or modify their schedule, and be aware of food requirements and possible triggers.
- Simply listening to your loved one is the best way to help them. As previously stated, in addition to the physical demands of Crohn’s disease, there can be a significant emotional toll. A trustworthy, encouraging, and patient listener can provide a secure space for your loved one to express and process feelings without fear of criticism.
- IBD can still be highly unpredictable, even with lifestyle modifications and treatment options. Be understanding if your friend has to cancel their entire event or arrives late. They probably would much rather be with you than be forced to stay at home due to uncomfortable symptoms.
- A chronic illness is certainly not a cause for shame, but that doesn’t mean you want everyone to know. Your companion may become even more uneasy and self-conscious due to some people’s assumptions or judgments about someone’s disease.
Participate in Crohn’s and Colitis Awareness Week Events
During Crohn’s and Colitis Awareness Week, you can participate in various in-person and virtual events to support the IBD community. From informative webinars to charity runs, these activities bring together advocates, families, and individuals in the fight against ulcerative colitis and Crohn’s disease.
If you prefer being active while raising awareness, consider joining a charity walk or run, such as the IBD Awareness Week event. Every step you take helps fund essential research for better treatments.
For those interested in learning more about IBD, virtual webinars and panel discussions, like the IBD Research Webinar, offer opportunities to hear from patients, researchers, and medical professionals about the latest treatment advancements.
Additionally, fundraising efforts encourage donations to support patient care and research. Attending these events, you help raise critical funds that improve therapies, increase public awareness, and provide much-needed support for those with IBD.
Conclusion
Managing Crohn’s disease and ulcerative colitis requires an understanding of these illnesses. Despite the difficulties, people can have happy lives with access to the appropriate information, resources, and care. Early symptom recognition, knowledge of various treatments, and an effective support system are key to controlling flare-ups and enhancing quality of life.
Remember that every path is different, whether you have Crohn’s disease or colitis or are supporting someone who does. Always consult your healthcare provider if you need personalized advice or feel overwhelmed—early intervention can make a difference in managing Crohn’s and colitis.
References
- https://crohnsandcolitis.org.uk/info-support/information-about-crohns-and-colitis/all-information-about-crohns-and-colitis/understanding-crohns-and-colitis/all-about-crohns-and-colitis
- https://crohnsandcolitis.ca/About-Crohn-s-Colitis/What-are-Crohns-and-Colitis
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/crohns-disease-and-ulcerative-colitis
- https://www.crohnscolitisfoundation.org/patientsandcaregivers/justlikeme/what-are-crohns-colitis
- https://www.niddk.nih.gov/health-information/digestive-diseases/crohns-disease/diagnosis
- https://crohnsandcolitis.org.uk/info-support/information-about-crohns-and-colitis/all-information-about-crohns-and-colitis/understanding-crohns-and-colitis/how-to-get-a-diagnosis
- https://www.mayoclinic.org/diseases-conditions/crohns-disease/symptoms-causes/syc-20353304
- https://my.clevelandclinic.org/health/diseases/9357-crohns-disease
- https://www.crohnscolitisfoundation.org/patientsandcaregivers/What-is-crohns-disease/treatment
- https://www.mayoclinic.org/diseases-conditions/crohns-disease/diagnosis-treatment/drc-20353309
- https://www.amg-gi.com/about
- https://crohnsandcolitis.org.uk/info-support/information-about-crohns-and-colitis/all-information-about-crohns-and-colitis/supporting-someone/supporting-someone-with-crohns-or-colitis
- https://www.crohnscolitisfoundation.org/supporting-someone-with-ibd
- https://www.crohnscolitisfoundation.org/events/ibd-pro-webinar-series-ibd-pain
- https://teamchallenge.crohnscolitisfoundation.org/
- https://crohnsandcolitis.org.uk/info-support/information-about-crohns-and-colitis/all-information-about-crohns-and-colitis/treatments?parent=23127&page=1&tags=&category=23127&sort=newest
In this Article