Affiliate Disclaimer
Some links in this article are affiliate links. We may earn a small commission if you make a purchase through these links, at no extra cost to you. We only recommend products we find useful to our readersFamily History and Diabetes Risk

Diabetes has been a global health problem across all ages. Though lifestyle factors contribute enormously towards its development in the form of diet and lack of exercise, family history would account for one of the most significant risk factors.
Knowing your risk and genetic predispositions might allow you to take extra care against diabetes. Both type 1 and type 2 diabetes have significant genetic components, but family history goes beyond inheritable genes. Shared family environments, habits, and health behaviors can also impact the risk of developing diabetes.
Understanding that family history plays a role will enable you to take active measures to reduce your chances of developing diabetes.
In this article, we’ll explore the impact of family history on diabetes risk and available tools to assess genetic predisposition. Whether you have a known family history or simply wish to understand your own risk, this article will arm you with knowledge to help protect your health.
The Genetic Connection to Diabetes
Diabetes has a considerable genetic contribution, and an individual’s risk of the disease is greatly influenced by family history. The degree of the link differs for different forms of diabetes:
Type 1 Diabetes and Genetics
Some genes, mainly those of the human leukocyte antigen complex, increase the risk for type 1 diabetes.
- Inheritance Pattern: A child whose parent or sibling has type 1 diabetes is more likely to be affected by the disease, but the overall risk is still quite low compared to inheriting type 2 diabetes.
- Gene-Environment Interaction: Environmental exposures, such as viral infections or early-life exposure to certain foods, may trigger the genetic susceptibility to type 1 diabetes.
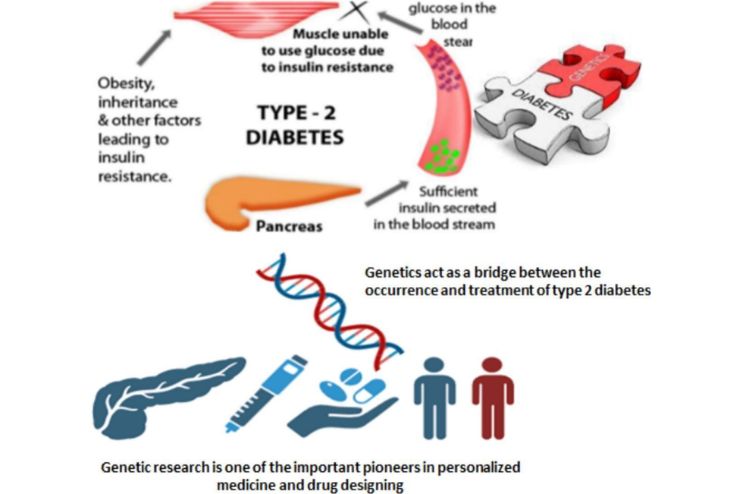
Type 2 Diabetes and Genetics
Genes have a strong influence on the development of Type 2 diabetes. High genetic predisposition is witnessed even more if a parent or sibling has type 2 diabetes.
- Polygenic Type: Unlike type 1, type 2 involves genetics working multi-fold through roles in insulin production and breakdown, glucose metabolism, and fat storage.
- Heritability: The heritability of type 2 diabetes is estimated to be between 30% and 70%, depending on genetic and lifestyle factors.
- Epigenetics: In addition to the inherited genes, epigenetic changes due to diet, physical activity, and other lifestyle factors can modify gene expression and increase the risk of developing type 2 diabetes.
Gestational Diabetes and Family History
Gestational diabetes, which occurs during pregnancy, is also influenced by genetics. Women with a family history of diabetes are at greater risk of developing gestational diabetes, which may also increase their risk of type 2 diabetes later in life.
Tools for Assessing Family History
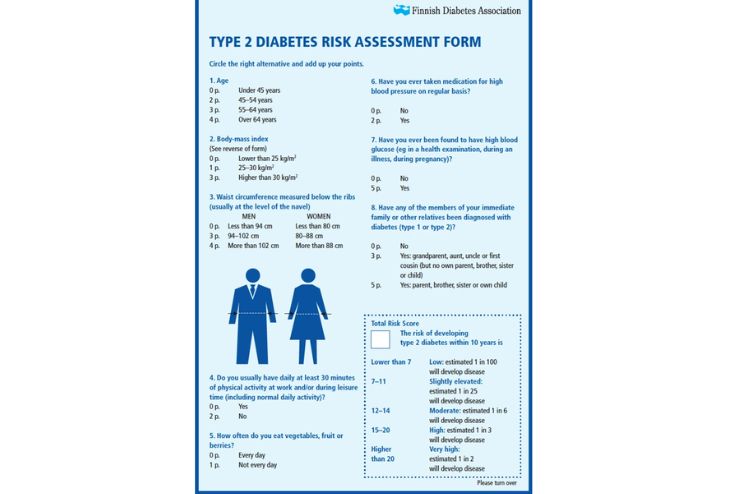
Knowing your family history is essential in determining your risk of developing diabetes. Gathering detailed information about your relatives’ health can help you work with healthcare providers to develop a tailored prevention or management plan.
Several tools and approaches can help evaluate family history effectively.
1. Family Health Questionnaires
A family health questionnaire is a structured form used to collect information about the medical history of immediate and extended family members. These questionnaires typically include questions about:
- Diagnosed conditions (e.g., diabetes, heart disease)
- Age of onset for chronic illnesses
- Lifestyle factors like diet, exercise, and smoking habits
Such forms provide a comprehensive view of hereditary risk factors and shared behaviors contributing to diabetes.
2. Family Medical History Tree
A family medical history tree or pedigree chart visually maps health conditions in a family of multiple generations.
- Use symbols and annotations to mark conditions, such as type 1 or type 2 diabetes, gestational diabetes, or other related disorders, including obesity or hypertension.
- Recording these patterns can identify clusters of diabetes or other metabolic conditions.
- Healthcare professionals commonly use these charts to identify patterns of heritability and determine the risk level.
3. Online Family Health Tools
Several online tools and websites allow a family health history to be documented and analyzed:
- My Family Health Portrait: This is an online tool developed by the U.S. Surgeon General. It allows individuals to enter, save, and share their family health information with providers.
- Genetic Testing Apps: Genetic testing services such as 23andMe or AncestryDNA provide some insights into predispositions to conditions like type 2 diabetes through DNA analysis.
4. Genetic Counseling and Testing
If there is a strong family history of diabetes or related conditions, genetic counseling may be recommended. A genetic counselor can:
- Assess the risk of inheriting diabetes
- Discuss genetic testing options
- Help interpret test results and develop a preventive care strategy
5. Health Records and Documentation
Collecting health records from family members and medical providers can provide invaluable details about:
- Laboratory results (e.g., blood glucose levels, HbA1c)
- Related diseases, including diagnosis of metabolic syndrome or gestational diabetes
- Treatment outcomes may reveal successful preventive interventions
6. Conversations with Family Members
Family history evaluation can be as easy and effective as having a straightforward discussion with family members
- Ask about chronic illnesses, including how long they have had such diseases, how they manage them, and if they have developed any.
- Ask about their eating habits or physical activity status.
- Be sensitive to confidentiality but explain the benefits that sharing information may have to family health.
7. Collaboration with Healthcare Providers
Healthcare providers are also responsible for assessing family history through analyzing the collected data and identifying risk factors. Further check-ups, blood tests, and screenings can help further fine-tune your knowledge of your health status in light of familial risk.
The Role of Epigenetics
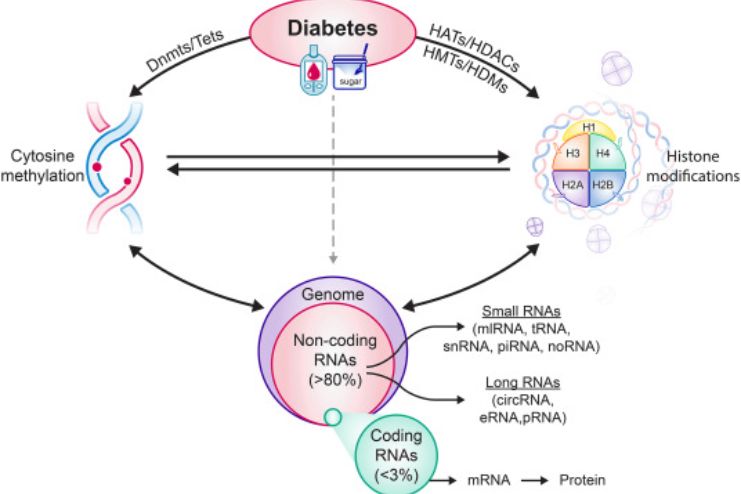
Epigenetics is a field of study that analyzes changes in gene expression without altering the DNA sequence. Understanding how family history can influence diabetes risk is crucial.
Genetics supplies the blueprint, but epigenetic mechanisms modify the way these genetic instructions are carried out, often through responses to environmental factors and lifestyle choices.
1. What Is Epigenetics?
Epigenetics is a biological process that controls how genes can be turned on or off. The processes include:
- DNA Methylation: Adding chemical groups (methyl groups) to DNA can silence or activate specific genes.
- Histone Modification: Changes in the proteins that DNA wraps around affect the tightness of genes or their accessibility for activation.
- Non-Coding RNA: Molecules that inhibit or enhance gene expression but do not change the DNA.
These alterations do not alter the DNA sequence; however, they may trigger the expression or suppression of genes involved in diabetes.
2. Epigenetics and Diabetes
Epigenetic alterations can impact susceptibility to type 1 and type 2 diabetes.
- Type 1 Diabetes: Although primarily an autoimmunity disease, an epigenetic event mediated by viral infections triggers immune responses against cells releasing insulin.
- Type 2 Diabetes: Obesity, diet, physical inactivity, and stress can cause epigenetic changes that lead to decreased insulin sensitivity or secretion.
These changes may explain why some people with a high genetic predisposition never get diabetes while others who have no family history do.
3. Transgenerational Epigenetics
Epigenetic changes can sometimes be inherited from one generation to another.
For instance, if a pregnant woman suffers from malnutrition or stress, epigenetic markers on the fetus might be altered. This increases the risk of developing diabetes when the child grows older.
On the other hand, the lifestyle and health condition of the father before conception may change the epigenetic profile of the sperm, thus affecting the epigenetic risk for metabolic conditions in the offspring.
4. Lifestyle Factors That Influence Epigenetics
Epigenetic mechanisms are highly influenced by environment and lifestyle choices, even among individuals with a family history of diabetes. These include the following:
- Diet: Consumption of whole foods, antioxidants, and nutrients promotes healthy gene expression. However, high sugar and processed food consumption may increase the risk of diabetes.
- Physical Activity: Exercising regularly can positively influence epigenetic markers associated with insulin sensitivity and metabolic health.
- Stress Management: Chronic stress can lead to epigenetic alterations that raise cortisol levels and compromise glucose metabolism.
- Exposure to Toxins: Smoking, pollution, and other chemicals have been associated with epigenetic changes related to diabetes.
5. Reversibility of Epigenetic Changes
The most exciting thing about epigenetics is that these changes are potentially reversible. Unlike genetic mutations, epigenetic modifications can usually be reversed through targeted lifestyle changes.
- Healthy Lifestyle Interventions: Adopting a balanced diet, regular exercise, and stress management techniques can reverse adverse epigenetic changes and thus reduce the risk of diabetes.
- Medication and Therapies: Specific drugs and experimental therapies are under research to target and modify harmful epigenetic changes in diabetes.
Conclusion
Therefore, it is important to understand the connection between family history and risk for diabetes to empower people to be proactive about prevention and management.
Genetics forms a basis for understanding susceptibility, but lifestyle and environmental factors through mechanisms like epigenetics determine whether that risk materializes into disease.
Risk reduction may occur by assessing family history, using genetic and epigenetic tools, and developing healthy habits. A well-balanced diet, regular exercise, and stress management may modify the expression of the genes related to diabetes and result in a diagnosis not consistent with their family history.
Ultimately, knowledge is power. Combining an awareness of familial risk with actionable lifestyle changes can help individuals take control of their health and work toward a future less burdened by diabetes. This underscores the importance of education, early intervention, and a personalized approach to diabetes prevention and care.
In this Article