Affiliate Disclaimer
Some links in this article are affiliate links. We may earn a small commission if you make a purchase through these links, at no extra cost to you. We only recommend products we find useful to our readersObsessive Compulsive Disorder (OCD) is a mental illness discovered by German neurologist and psychiatrist Wilhelm Griesinger in 1868. After his notes, on OCD, where he referred to it as “racking one’s brain, questioning illness”, the modern psychologists who have given new way to treatment of OCD, after Sigmund Freud’s technique-psychoanalysis- has been Karl Freidriech Otto Westphal and Pierre Janet. Westphal describes OCD as “intrusive thoughts” that are beyond the patients’ control. Janet separated OCD from neurasthenia.
The causes of OCD are unknown, mostly said to be caused by genetic and environmental factors like somebody in the family having anxiety-related disorders or OCD. It can also be triggered by a traumatic event like child abuse. People with OCD face a high suicide risk. Treatment is now available but there is no way to cure OCD completely. It can stay for a lifetime.
The main point is that obsessive and compulsive behaviours are two separate aspects in the person. Obsessions are mostly because of genetic and hereditary factors and compulsions are known to be caused by learned behaviours which become habits. The classification has been attenuated based on the symptoms seen in various individuals reporting certain traits like washing hands continuously after coming back home from outside and staying indoors, which would be characterised as a compulsion. These are repetitive actions like “tics” that an OCD person carries out involuntarily to get rid of the anxiety caused by not washing hands.
OCD usually occurs in individuals from before the age of 20 to 30. Very rarely would OCD symptoms appear after the age of 35. Mostly OCD occurs equally amongst men and women. In the world, OCD occurs in a person’s life at the rate of 2.3 people at some point at the yearly rate of 1.2 percent. It is common to find comorbidity in people with OCD. The comorbidity symptoms in OCD symptoms and OCD behaviour, for example, OCD and Attention Deficit Hyperactivity Disorder (ADHD) is as high as 51 percent in the world.
What is OCD?
 According to psychology, psychiatry, and neuroscience was able to identify OCD as a common condition when an individual repeated certain actions with a rational of his/her own. But this rationale is not useful -like always checking the door knob to see if it is locked, or cleaning shelves every 5 to 10 minutes- using more than an hour to just repeat the same action every day which disrupts normal life, can be called OCD.
According to psychology, psychiatry, and neuroscience was able to identify OCD as a common condition when an individual repeated certain actions with a rational of his/her own. But this rationale is not useful -like always checking the door knob to see if it is locked, or cleaning shelves every 5 to 10 minutes- using more than an hour to just repeat the same action every day which disrupts normal life, can be called OCD.
OCD can be because of childhood abuse, severe past trauma, or repressed memory, but still as per official sense of the disorder according to Diagnostic and statistical manual of mental disorders : DSM-5 (R) there is no obvious cause of OCD known. Patients’ usually come to the doctors’ because of their own realisation or because a family member or friend observes OCD-like behaviour in them.
8 Types of OCD?
There are many types of OCD based on pattern recognition in various patients over the years now. Here are common 7 types of OCD recognised largely:
1. Checking:
 Seeing if the window is open or closed, or a door knob for the same reason, is it locked or not is a common “checking” symptom of OCD. There is a fear that the door or window may be open and hence the OCD patient needs to close it immediately. This he or she does repeatedly more than three times and cannot rest for hours thinking obsessively about the window or the door knob. If the person does this in a situation, like in his or her workplace or family get-together, he or she may be a source of laughter, embarrassment or concern. This is just one example of how OCD can disrupt normal life of the person.
Seeing if the window is open or closed, or a door knob for the same reason, is it locked or not is a common “checking” symptom of OCD. There is a fear that the door or window may be open and hence the OCD patient needs to close it immediately. This he or she does repeatedly more than three times and cannot rest for hours thinking obsessively about the window or the door knob. If the person does this in a situation, like in his or her workplace or family get-together, he or she may be a source of laughter, embarrassment or concern. This is just one example of how OCD can disrupt normal life of the person.
2. Contamination:
 Contamination of germs, is the most common type of OCD. There is a fear in the OCD patient that they may be carriers of germs, or somebody or something else might be carrying germs that they might contract a fatal disease from. This thought causes so much anxiety in them that they land up cleaning and washing themselves up for hours in a day. Wasting time. In colloquial language, these people are also called “washers”.
Contamination of germs, is the most common type of OCD. There is a fear in the OCD patient that they may be carriers of germs, or somebody or something else might be carrying germs that they might contract a fatal disease from. This thought causes so much anxiety in them that they land up cleaning and washing themselves up for hours in a day. Wasting time. In colloquial language, these people are also called “washers”.
3. Mental Contamination:
 There is a feeling in the OCD person that they are contaminated, or somebody or something else is “magically” and “metaphysically” contaminated. In this case they have a belief that this contamination is because of evil or impure thoughts they harbour. This can cause extreme anxiety and distress in the OCD patient. They have a mental picture that somebody is spreading negativity. And this can perhaps initiate a series of “irrational” behaviours in the OCD patient who would be trying to get rid of the mental contamination.
There is a feeling in the OCD person that they are contaminated, or somebody or something else is “magically” and “metaphysically” contaminated. In this case they have a belief that this contamination is because of evil or impure thoughts they harbour. This can cause extreme anxiety and distress in the OCD patient. They have a mental picture that somebody is spreading negativity. And this can perhaps initiate a series of “irrational” behaviours in the OCD patient who would be trying to get rid of the mental contamination.
4. Hoarding:
 It is the need to have items of no value is close possession without any strong reason, for example, a cardboard box, an old cup or flyers that fill up living space. Hoarding can occur because of excessive buying. And what they buy usually seems not proper to people around the hoarder. Hoarding in OCD patients can lead to disastrous conditions where they live among old things, believing it to be antique and valuable, they cause depression in others who live around them. They themselves live in hazardous conditions where they can neither throw away the item nor are able to maintain their quality.
It is the need to have items of no value is close possession without any strong reason, for example, a cardboard box, an old cup or flyers that fill up living space. Hoarding can occur because of excessive buying. And what they buy usually seems not proper to people around the hoarder. Hoarding in OCD patients can lead to disastrous conditions where they live among old things, believing it to be antique and valuable, they cause depression in others who live around them. They themselves live in hazardous conditions where they can neither throw away the item nor are able to maintain their quality.
5. Ruminations:
 Spending an inordinate amount of time trying to figure out a theme or concept which is of no use to anybody, but feeling that the result of being able to articulate it will change the world is the feeling an OCD person gets from his thoughts. They can ruminate about philosophy or anything. This causes them to regurgitate food after a meal. This behaviour can get too aggressive as well. Due to this they suffer from abdominal pain, nausea and unintentional weight loss.
Spending an inordinate amount of time trying to figure out a theme or concept which is of no use to anybody, but feeling that the result of being able to articulate it will change the world is the feeling an OCD person gets from his thoughts. They can ruminate about philosophy or anything. This causes them to regurgitate food after a meal. This behaviour can get too aggressive as well. Due to this they suffer from abdominal pain, nausea and unintentional weight loss.
6. Intrusive Thoughts:
 There may be a memory of a traumatic event, or imaginary event obstructing a person’s daily life while they are working. For example, sexual encounters with a family member or a morally wrong thought which keeps coming into mind, involuntarily and is unstoppable by the OCD patient, with their own will power. In such a case they go through immense lack of sleep and anxiety which affects their health and being.
There may be a memory of a traumatic event, or imaginary event obstructing a person’s daily life while they are working. For example, sexual encounters with a family member or a morally wrong thought which keeps coming into mind, involuntarily and is unstoppable by the OCD patient, with their own will power. In such a case they go through immense lack of sleep and anxiety which affects their health and being.
7. Symmetry and Orderliness:
 Arranging things in order of height, weight or MRP can be a type of OCD. If it is your job to put things in order then this is not OCD. But if you happen to find somebody or yourself arranging things in order of height in a shopping mall without any reason, then this might be a time to seek help. Counting, tapping or tugging things to make sure they are in some kind of symmetry is OCD.
Arranging things in order of height, weight or MRP can be a type of OCD. If it is your job to put things in order then this is not OCD. But if you happen to find somebody or yourself arranging things in order of height in a shopping mall without any reason, then this might be a time to seek help. Counting, tapping or tugging things to make sure they are in some kind of symmetry is OCD.
8. Trigger:
 Trigger is a general word for understanding that OCD occurs from doubt or harm. These are the main triggers. If a person feels that every action entails some harm he or she may not stop checking to make it right. Also, if the person feels strongly a doubt that the origin of the universe has been misinterpreted for thousands of years, he or she may try to solve the puzzle and waste days, or months trying to solve it, if there is nobody to care about them. Again, if you are a philosopher, and thinking of the origin of the universe is going to fetch some benefit to you and others around you, it is not OCD.
Trigger is a general word for understanding that OCD occurs from doubt or harm. These are the main triggers. If a person feels that every action entails some harm he or she may not stop checking to make it right. Also, if the person feels strongly a doubt that the origin of the universe has been misinterpreted for thousands of years, he or she may try to solve the puzzle and waste days, or months trying to solve it, if there is nobody to care about them. Again, if you are a philosopher, and thinking of the origin of the universe is going to fetch some benefit to you and others around you, it is not OCD.
6 changes in life of an OCD patient?
 Once you know you have OCD it is easier to stop the compulsive behaviour. Note that OCD is not the same as Obsessive Compulsive Personality Disorder (OCPD), which can include bipolar mood disorder and it is characterised by excessive need for orderliness, neatness and perfectionism. It has overlapping symptoms. But being neat and tidy is neither sign of OCD or OCPD.
Once you know you have OCD it is easier to stop the compulsive behaviour. Note that OCD is not the same as Obsessive Compulsive Personality Disorder (OCPD), which can include bipolar mood disorder and it is characterised by excessive need for orderliness, neatness and perfectionism. It has overlapping symptoms. But being neat and tidy is neither sign of OCD or OCPD.
OCD is the involuntary need to do repetitive actions which can disrupt normal life. On the other hand, OCPD includes knowing the actions have aim or purpose and therefore to the patient it is normal.
At some point, an OCD person does realise that they are doing something too much for it to be normal. It is important to recognise symptoms in OCD to stop the compulsive actions. They are:
1. Identify actions with extra attention:
 Once you are checking, ruminating, or washing yourself because of contamination. You can start by taking the first step that is making a mental note, then a written note of the action you have taken towards avoiding the supposed danger to avoid wasting your time doing the action repetitively. Therefore, when the urge to do the action arises again, you can review your actions which will cause much less distress to you.
Once you are checking, ruminating, or washing yourself because of contamination. You can start by taking the first step that is making a mental note, then a written note of the action you have taken towards avoiding the supposed danger to avoid wasting your time doing the action repetitively. Therefore, when the urge to do the action arises again, you can review your actions which will cause much less distress to you.
2. Resist compulsions:
 Make a list of things that frighten you or cause you anxiety on the basis of stress levels. These stress levels should be marked according to your level of anxiety and distress a causal trigger has on you. You have to work yourself up the ladder by exposing yourself to the trigger. For example, if you wash your hands because you have come from outside and germs are your “extreme” anxiety, keep them last. If you have to wash hands continuously with soap, then point one should be not using soap once after eating your food. The number 1 obsession will be the least anxiety provoking. Surely, everyday practice of resisting compulsion will bring you to a normal behaviour pattern with 6 weeks to 24 weeks.
Make a list of things that frighten you or cause you anxiety on the basis of stress levels. These stress levels should be marked according to your level of anxiety and distress a causal trigger has on you. You have to work yourself up the ladder by exposing yourself to the trigger. For example, if you wash your hands because you have come from outside and germs are your “extreme” anxiety, keep them last. If you have to wash hands continuously with soap, then point one should be not using soap once after eating your food. The number 1 obsession will be the least anxiety provoking. Surely, everyday practice of resisting compulsion will bring you to a normal behaviour pattern with 6 weeks to 24 weeks.
3. Challenge yourself:
 Once you know your obsessions and compulsions journaling them down will reduce the anxiety. One by one give yourself “worry periods”. In this worry period you will think about your obsessive thoughts, it can be anything- like having sex with a stranger. Let yourself be and make notes of your exact feelings and compulsive actions that you think will relieve you of the anxiety. You can have one or two hours of “worry period” everyday. Once you give yourself designated hours to worry about your obsessions, you can do useful activities and rest for the day.
Once you know your obsessions and compulsions journaling them down will reduce the anxiety. One by one give yourself “worry periods”. In this worry period you will think about your obsessive thoughts, it can be anything- like having sex with a stranger. Let yourself be and make notes of your exact feelings and compulsive actions that you think will relieve you of the anxiety. You can have one or two hours of “worry period” everyday. Once you give yourself designated hours to worry about your obsessions, you can do useful activities and rest for the day.
4. Reach out:
 If you are not ready for taking matters in your own hand there is no harm in reaching out to friends and family. Going to a therapist or a psychiatrist would be the best choice. If you delay your treatment to OCD, it might get worse. Some undiagnosed cases of OCD stay for a lifetime causing immense unease and work life imbalance. Join a community of OCD patients who can talk and discuss with you their own struggles. You don’t have to feel alone.
If you are not ready for taking matters in your own hand there is no harm in reaching out to friends and family. Going to a therapist or a psychiatrist would be the best choice. If you delay your treatment to OCD, it might get worse. Some undiagnosed cases of OCD stay for a lifetime causing immense unease and work life imbalance. Join a community of OCD patients who can talk and discuss with you their own struggles. You don’t have to feel alone.
5. Stress management:
 If you are feeling helpless or powerless because of your obsessions and compulsions, take your time to relax too. There are various ways to manage stress, one of them is talking to people about your feelings and letting go of all that you have stored in. This can be called “emotional flooding” and is also used as a therapy treatment to reduce anxiety from OCD.
If you are feeling helpless or powerless because of your obsessions and compulsions, take your time to relax too. There are various ways to manage stress, one of them is talking to people about your feelings and letting go of all that you have stored in. This can be called “emotional flooding” and is also used as a therapy treatment to reduce anxiety from OCD.
6. Lifestyle changes:
 Including exercise, yoga and meditation in your daily life and making good food choices may also completely change your OCD symptoms and make your focus on things which can transform your life in a good way. Don’t think too much about what to do, just do them in the designated hours of the day.
Including exercise, yoga and meditation in your daily life and making good food choices may also completely change your OCD symptoms and make your focus on things which can transform your life in a good way. Don’t think too much about what to do, just do them in the designated hours of the day.
What causes OCD?
 There is no exact cause of OCD. Research shows that OCD is caused by genetic factors and also neurological factors. In genetic factors, it is because somebody in the family or even extended family may have OCD or associated disorders which are passed on from generations. It is also true that daily stress from various activities can cause OCD. It could be that the patient had overprotective parents who did not offer much care.
There is no exact cause of OCD. Research shows that OCD is caused by genetic factors and also neurological factors. In genetic factors, it is because somebody in the family or even extended family may have OCD or associated disorders which are passed on from generations. It is also true that daily stress from various activities can cause OCD. It could be that the patient had overprotective parents who did not offer much care.
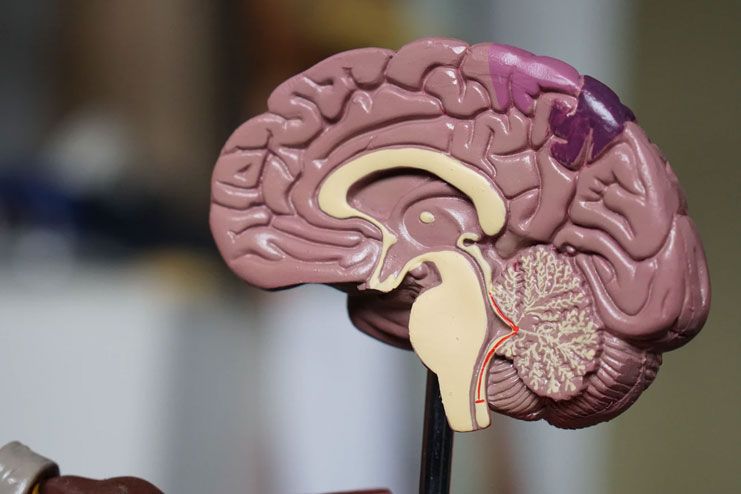
In neurological factors, it is known that serotonin plays a huge role in OCD. OCD patients usually lack communication in the front lobe cortex and the deeper areas of the brain, which is carried out by serotonin. Structural abnormalities in the brain have also been found in OCD patients.
Pediatric Autoimmune NeuroPsychiatric Disorder Associated with Streptococcal Infections (PANDAS) is also an OCD, but it occurs in children because of streptococcus infection in early age. The symptoms are like OCD and are visible overnight after infection. This has a severe impact on the child’s life.
8 risk factors of OCD?
 OCD is mostly related to a historical event or reason.
OCD is mostly related to a historical event or reason.
- Stressful events in the past, for example, an accident like a house catching fire.
- The patient has a clear memory of child abuse which assures them that the evil thoughts they are having have reason.
- History of skin infections may cause an OCD patient to pick their skin so much that they have scars, scratches and scabs all over their body.
- Immense anxiety of losing weight or believing that they need to lose weight for their own good can lead to eating disorders.
- Attention Deficit Hyperactivity Disorder (ADHD) While being focused on the obsession or intrusive thought, the OCD patient may not be able to concentrate on their work through which they make an earning. Symptoms are cutting in a conversation continuously when others are talking.
- Tourette syndrome is common among severe cases of OCD, this constitutes sniffing, blinking, grimacing, head movements and throat clearing.
- Social anxiety is also an associated risk factor with OCD when people fear going out completely in fear of catching germs, or that they have forgotten to lock the doors previously so they may as well just sit at home.
- Major Depressive Disorder is caused because of over thinking of their own condition and not being able to mix with the crowd as much as others do.
How to Diagnose OCD?
 OCD can be diagnosed mainly by paying attention to the symptoms. People with OCD exhibit very specific symptoms including repetitive actions fearing loss. They have anxiety if they don’t complete the action- which is called a compulsive behaviour.
OCD can be diagnosed mainly by paying attention to the symptoms. People with OCD exhibit very specific symptoms including repetitive actions fearing loss. They have anxiety if they don’t complete the action- which is called a compulsive behaviour.
- OCD can be diagnosed through brain scan, X-ray, or physical symptoms of scratching body parts with nails.
- Using the Diagnostic and Statistical Manual of Mental Disorders (DSM) (R) by American Psychiatric Association is one way of diagnosing OCD patterns.
- Psychological evaluation by a psychiatrist, psychologist, social worker or certified friend is also a way to get OCD diagnosed.
5 best ways to treat OCD?
1. Cognitive Behaviour Therapy (CBT):
 This includes exposure and response prevention. You expose the patient to his fear or obsession, for example, coming out of the washroom. The ritual obsession is that he or she would want to wash his or her hands because they want to get rid of the germs from the toilet.
This includes exposure and response prevention. You expose the patient to his fear or obsession, for example, coming out of the washroom. The ritual obsession is that he or she would want to wash his or her hands because they want to get rid of the germs from the toilet.
But they do it so often that they land up wasting hours. So the response would be to resist the urge to wash hands more than once. The practice of doing this through interventions is called CBT. This works well on most patients of OCD but not all and has limited effect on the individual.
2. Deep brain stimulation (DBS):
 Patients who do not respond well to medication and therapy opt for DBS. It has recently been approved by the Food and Drug Administration (FDA) as Humanitarian Device Exemption (HDE). This is not possible for everybody to go for this procedure. DBS is an invasive technique as it requires surgery.
Patients who do not respond well to medication and therapy opt for DBS. It has recently been approved by the Food and Drug Administration (FDA) as Humanitarian Device Exemption (HDE). This is not possible for everybody to go for this procedure. DBS is an invasive technique as it requires surgery.
In DBS, electrodes are placed in the brain of the patient and the wires of the electrode are fixed to pulse regulators in the body and electric simulation is passed through the wires to the brain. Only experts and experienced DBS professionals can carry out this process because the quantity of stimulation to be passed through the wire is specific to each patient.
3. Transcranial magnetic stimulation (TMS):
 TMS is a non-invasive method to treat OCD. It corrects the communication between different neurons in the neuron-network. It is an FDA approved method. A coil is placed over 5X2’’ above the head targeting a region of the head. The wires are connected to a stimulation device which passes electricity through the skin, muscle and bone and causes the neurons to fire. This is done five days a week and takes about 20-40 minutes each session.
TMS is a non-invasive method to treat OCD. It corrects the communication between different neurons in the neuron-network. It is an FDA approved method. A coil is placed over 5X2’’ above the head targeting a region of the head. The wires are connected to a stimulation device which passes electricity through the skin, muscle and bone and causes the neurons to fire. This is done five days a week and takes about 20-40 minutes each session.
TMS targets three main areas of the brain to restructure neural networks 1) Dorsolateral prefrontal cortex, 2) Orbitofrontal cortex (OFC) and 3) Pre-supplementary Motor Area (P-SMA).
4. Selective serotonin re-uptake inhibitors medication:
 SSRIs and the drug clomipramine are the most commonly used medications for OCD. These medications increase the concentration of serotonin, a neurotransmitter, in the brain. Patients with OCD typically take 10 to 12 weeks to respond.
SSRIs and the drug clomipramine are the most commonly used medications for OCD. These medications increase the concentration of serotonin, a neurotransmitter, in the brain. Patients with OCD typically take 10 to 12 weeks to respond.
Fluoxetine (Prozac), fluvoxamine (Luvox), paroxetine (Paxil), citalopram (Celexa), escitalopram (Lexapro), and sertraline (Zoloft) are some common SSRI. They are generally preferred over clomipramine in treating OCD.
5. Intensive OCD outpatient and residential treatment programs:
 There are several centres in mental hospitals in every state which look into intensive programs designed to cure OCD. There is a rehab and Equine Assisted Activity Program (EAA) specializing in OCD and anxiety disorders in these centres. These have experts catering to patient needs by having a history of their hoarding disorder, phobia track etc.
There are several centres in mental hospitals in every state which look into intensive programs designed to cure OCD. There is a rehab and Equine Assisted Activity Program (EAA) specializing in OCD and anxiety disorders in these centres. These have experts catering to patient needs by having a history of their hoarding disorder, phobia track etc.
Diseases an OCD person can get over easily?
 There is no full and final cure for OCD but there are various physical effects of OCD one can get over easily like scabies and infections from scratching with nails. Depression and anxiety are associated disorders and the patient can get over these substantially through medication and psychotherapy. OCD patients with substance abuse reform fast with rehab in psychiatric hospitals.
There is no full and final cure for OCD but there are various physical effects of OCD one can get over easily like scabies and infections from scratching with nails. Depression and anxiety are associated disorders and the patient can get over these substantially through medication and psychotherapy. OCD patients with substance abuse reform fast with rehab in psychiatric hospitals.
Conclusion
Till now, there is no known foundational OCD cause. It is caused by genetic and environmental factors. OCD is a mental illness caused in children, men and women of age group 10-30. This can lead to anxiety disorder and depression. The patient in OCD obsesses over a thought and carries out compulsive behavioural actions which are harmful to them or others. OCD symptoms include scratching one’s own skin thinking that there is a tic on their skin because they touched a dog. Or, it can also be that they cannot stop washing their hands after coming home from outside. OCD risk factors can be horrible, include high suicide risk. OCD treatment is now available, but there is no way to be completely cured of OCD.
Recommended:
- OCD Treatment: What You Should Know?
- 7 Ways For Overcoming ROCD (Relationship OCD) For A Happier Relationship
- 17 Alarming Signs That You Are Suffering From Obsessive Compulsive Disorder
In this Article


















