AI Contribution
At HealthSpectra, we may use AI to refine grammar and structure, but every piece is shaped, checked, and approved by real people, our expert writers and editors, to ensure clarity, credibility, and care. Learn more..Affiliate Disclaimer
Some links in this article are affiliate links. We may earn a small commission if you make a purchase through these links, at no extra cost to you. We only recommend products we find useful to our readersDiabetes mellitus is a metabolic disorder that affects millions worldwide. It is primarily characterized by hyperglycemia due to either reduced insulin production or impaired insulin utilization by the body. Despite the significant focus on insulin in diabetes discussions, hormonal imbalances beyond insulin play a crucial role in the effectiveness of the treatment.
Understanding these hormonal imbalances is fundamental to understanding the complexities of diabetes, effective treatment strategies, and proper diabetes management.
This article explores the critical hormonal imbalances in diabetes, their physiological roles, and their implications for metabolic health.
Insulin and Its Role in Diabetes

Insulin is a peptide hormone secreted by beta cells in the pancreas. Its main role in humans is to ensure that blood glucose remains at a homeostasis level. Other roles of insulin include stimulating the intake of glucose into cells for energy use, encouraging the storage of glucose as glycogen in the liver and muscles, and stimulating fat storage.
The role of insulin in diabetes mainly falls into two major categories: Type 1 and Type 2 diabetes.
- Type 1 Diabetes: It is an autoimmune condition that destroys the beta cells responsible for insulin production. This leads to an absolute deficiency of insulin. Survival and maintenance of normal blood glucose levels depend on the exogenous supply of insulin for patients suffering from type 1 diabetes.
- Type 2 Diabetes: In this more prevalent type of diabetes, the body initially produces insulin but becomes resistant to its effects over time. It requires more insulin to accomplish a blood-glucose-lowering effect. Over time, pancreatic beta cells can become depleted, resulting in diminished insulin production.
Mechanisms of Insulin Resistance: Obesity, lack of physical activity, genetic predisposition, and some hormonal imbalances are factors involved with insulin resistance. Free fatty acids and inflammatory cytokines released by excess fat tissue in obesity interfere with insulin signaling pathways, thus enhancing insulin resistance.
Counter-Regulatory Hormones
Your body balances its blood glucose levels through hormonal balance. Some counter-regulatory hormones work against insulin function and increase glucose levels.
-
Glucagon:
This hormone is secreted by the alpha cells of the pancreas and is responsible for increasing blood glucose. Glucagon stimulates gluconeogenesis, which is the generation of glucose from various non-carbohydrate sources, and glycogenolysis, which is the breakdown of glycogen into glucose.
In diabetes, glucagon secretion can become unbalanced, leading to increased glucose production associated with hyperglycemia. Even in hyperglycemia, glucagon levels remain inappropriately elevated in type 2 diabetes, contributing to further blood sugar increases.
-
Cortisol:
Cortisol release is linked to the adrenal glands and facilitates the body’s response to stress. Cortisol can increase gluconeogenesis and reduce the action of insulin, thereby increasing blood glucose levels.
Prolonged chronic stress could lead to chronically elevated levels of cortisol, which can also strengthen insulin resistance and increase the tendency to develop type 2 diabetes.
Cushing’s Syndrome, resulting from too much cortisol, is associated with considerable weight gain, diminished insulin sensitivity, and increased incidence of diabetes.
-
Epinephrine (Adrenaline):
In acute stress, epinephrine mobilizes stored energy, thereby raising blood glucose. In chronic stress, epinephrine periodically swamps body cells, leading to hyperglycemia.
-
Growth Hormone:
Growth hormone is released from the pituitary gland and is associated with making the body resistant to insulin and breaking down fats. Excess growth hormone is considered to increase blood sugar, which is one of the causes of diabetes.
The pituitary gland exceeds the production of growth hormone in acromegaly, which is associated with increased insulin resistance and type 2 diabetes.
Appetite/Weight Regulation-Linked Hormones

There are several hormones that regulate appetite and have the potential to greatly affect body weight and risk for diabetes. Of these, the most important is leptin, which is produced by adipose or fat tissue and represents a key role in making you feel full and also in the regulation of energy expenditure.
In obese individuals, the body often becomes leptin-resistant, unable to respond properly to the leptin signals, causing greater hunger and potential weight gain, both of these being significant risks for type 2 diabetes.
-
The Interrelation of Leptin and Insulin:
Leptin and insulin work closely together, as they influence each other’s signaling pathways. Dysregulated leptin signaling is commonly observed in individuals with insulin resistance, which further complicates weight management and metabolic health. Insulin resistance, in turn, can exacerbate leptin resistance, creating a vicious cycle that increases the risk of diabetes.
-
Ghrelin – The Hunger Hormone:
Ghrelin is secreted from the stomach and enhances appetite. Elevated ghrelin levels will increase overeating instances and contribute to obesity. This subsequently increases the risk for both insulin resistance and diabetes.
-
Adiponectin – A Protective Horome:
This hormone, secreted by adipose tissue, has anti-inflammatory and insulin-sensitising properties. Low levels of adiponectin are associated with obesity and type 2 diabetes. Thus, it is also linked to metabolic health.
In obese individuals, adiponectin resistance can occur, further impairing insulin sensitivity and promoting the development of metabolic disorders, including diabetes. This resistance contributes to a disrupted metabolic balance, making it harder for the body to regulate blood sugar levels and weight effectively.
Thyroid Hormones
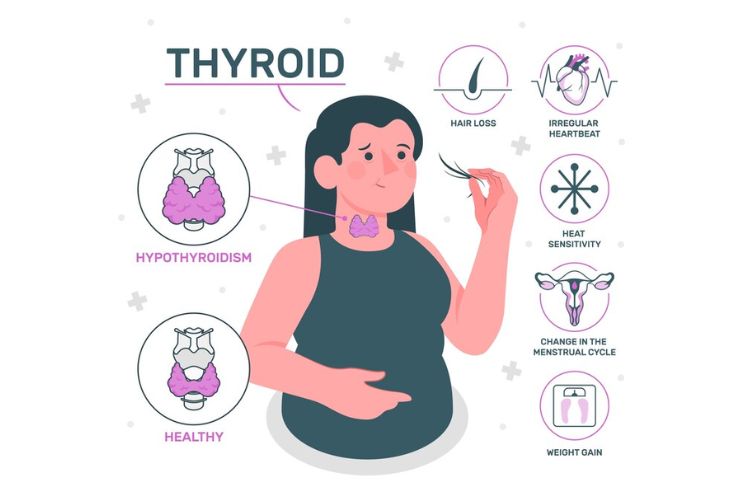
The thyroid gland plays a crucial role in regulating metabolism by producing thyroid hormones that influence various bodily functions, including glucose metabolism. Disruptions in thyroid hormone levels can significantly affect the body’s ability to manage blood sugar and may contribute to the development of diabetes.
Below are the key thyroid disorders and their relationship with glucose metabolism:
- Hypothyroidism:
When the levels of thyroid hormones are lower than the normal value, sensitivity to insulin decreases, and blood sugar levels tend to increase. People with hypothyroidism are likely to become more vulnerable to type 2 diabetes.
- Hyperthyroidism:
In contrast, hyperthyroidism occurs when the thyroid produces an excess of thyroid, resulting in increased metabolic activity. This often leads to temporary weight loss and heightened energy expenditure. However, prolonged hyperthyroidism can disrupt glucose metabolism and impair insulin action, leading to dysglycemia (abnormal blood sugar levels). Over time, this can increase the risk of developing diabetes-related complications.
- Thyroid Hormones and Metabolism:
Thyroid hormones are vital for normal metabolic activities. The absence of thyroid hormones—as seen in hypothyroidism—can lead to weight gain, particularly an increase in body fat. This can exacerbate insulin resistance, a condition where the body’s cells become less responsive to insulin, further complicating glucose regulation and increasing the likelihood of developing diabetes.
- Thyroid Function and Diabetes Management:
Diabetes not only affects glucose metabolism but can also interfere with thyroid function. For instance, individuals with diabetes may be more prone to developing hypothyroidism, which can further alter glucose metabolism and hinder diabetes management. Thus, thyroid health plays an important role in the overall management and progression of diabetes.
Sex Hormones
The sex hormones, which include mainly estrogen and testosterone, are associated directly with glucose metabolism, and an imbalance in these poses a risk of developing diabetes:
- Estrogen: This female sex hormone protects women against type 2 diabetes. It has protective effects for premenopausal women, but during menopause, decreased estrogen leads to increased fat tissue in the abdomen and promotes insulin resistance.
- Menopause and Diabetes Risk: Transition to menopause is risky due to a gradual change in the hormonal status, promoting weight gain and metabolic dysfunction, which leads to type 2 diabetes.
- Testosterone: Low levels of testosterone in males have been associated with several increased risks for type 2 diabetes. A testosterone deficiency results in insulin resistance and excess body fat, especially around the abdominal regions.
- Androgens: Testosterone replacement therapy improves the sensitivity towards insulin in men with low testosterone levels and can improve their metabolic status.
Conclusion
Hormones in the diabetes pathophysiology regulate sensitivity to insulin, appetite, and metabolic state. Understanding these intricate hormonal interactions is important for determining more effective plans for preventing and managing diabetes.
Thus, there is a more comprehensive approach to everything from insulin levels to other hormonal influences regarding diabetes patients. Research regarding the impact of hormones on diabetes, therefore, greatly helps us understand and care for T2D.
Correcting hormonal imbalances will improve the quality of life in diabetic patients and may also reduce the prevalence of diabetes in the population.
In this Article





















