AI Contribution
At HealthSpectra, we may use AI to refine grammar and structure, but every piece is shaped, checked, and approved by real people, our expert writers and editors, to ensure clarity, credibility, and care. Learn more..Affiliate Disclaimer
Some links in this article are affiliate links. We may earn a small commission if you make a purchase through these links, at no extra cost to you. We only recommend products we find useful to our readersType 1 Diabetes requires being in management mode always, and unlike type 2 diabetes, the prime cause of T1D is not insulin resistance; instead, it is autoimmune that destroys the cells located in the pancreas. It is a disease where patients have to continue taking insulin injections.
Keeping the blood sugar level balanced with daily management is sometimes unavoidable. Still, knowing the long-term health-related implications of T1D helps you better prepare and act correctly. This awareness, coupled with regular medical treatment, minimizes the complications and contributes to a healthier, wealthier life for the T1D sufferer.
Please read our “Understanding Type 1 Diabetes” article, which provides a comprehensive overview of the causes, symptoms, and management of this autoimmune condition.
Long-Term Health Challenges of Type 1 Diabetes
Type 1 diabetes (T1D) leads to several physical complications in different parts of the body. Proper glycemic control would help avoid these complications because there is still significant long-term risk even with excellent control.
The most prevalent complication of T1D is diabetic retinopathy, which is damage caused by high blood glucose to the blood vessels within the retina. This causes blindness and visual impairments. Other complications may lead to cataracts, diabetic macular edema, and nerve damage that impacts eye health.
1. Diabetic Neuropathy
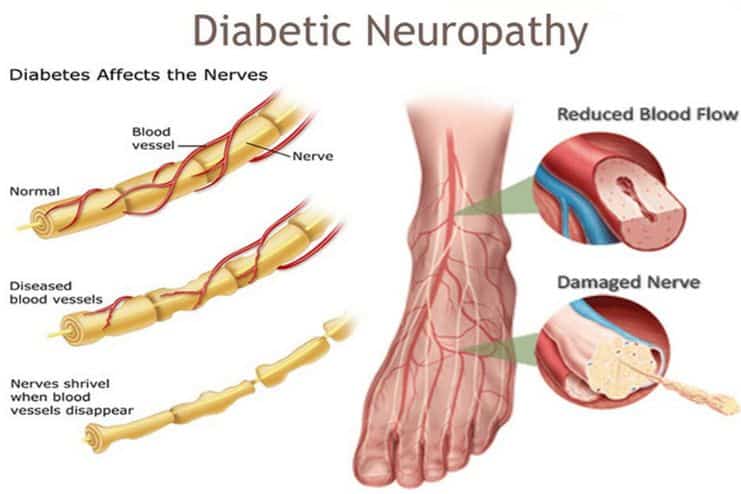
Diabetic neuropathy affects approximately 50% of individuals with diabetes. This condition arises from prolonged hyperglycemia, which damages neurons, particularly in the limbs and other areas like the armpits. It causes various symptoms, including pain, numbness, tingling, and reduced sensation in the affected regions.
In severe cases, diabetic neuropathy can result in significant loss of mobility, as individuals may not feel injuries. This lack of sensation increases the risk of infections and other serious complications.
2. Kidney Disease
This condition is commonly referred to as diabetic nephropathy. It occurs when the kidneys are damaged due to prolonged exposure to high blood sugar levels as they work to filter the excess glucose from the blood over many years.
Over time, this damage reduces the kidneys’ efficiency in filtering waste from the bloodstream. In advanced stages, dialysis or even a kidney transplant may become necessary.
3. Cardiovascular Risks
Individuals with T1D are much more likely to develop heart disease and stroke because of how diabetes affects the blood pressure and cholesterol of an individual. High glucose in the blood causes hardening of the arteries, among other cardiovascular complications.
4. Gastrointestinal Problems

Diabetes can also influence the digestive system, causing gastroparesis, constipation, or diarrhea. The problems result from nerve damage that impacts the stomach and intestines’ functioning, complicating digestion and nutrient absorption.
5. Complications in Pregnancy
Pregnancy complications for women with type 1 diabetes (T1D) can include miscarriage, pre-eclampsia, and fetal abnormalities. Managing T1D during pregnancy requires close monitoring and careful control of blood glucose levels to reduce risks and safeguard the health of both the mother and the baby.
Also Read: Unravelling the Causes of Gestational Diabetes During Pregnancy
6. Mental Health and Cognitive Impairment
The presence of diabetes increases the risk of developing depression, which can further complicate disease management. Additionally, research has shown that type 1 diabetes (T1D) may increase the risk of cognitive decline and susceptibility to dementia later in life.
Also Read: Practical Strategies to Prioritize Mental Wellness
Conclusion
Type 1 diabetes (T1D) presents significant long-term management challenges that go beyond physical health, as it can profoundly affect quality of life. Intensified insulin therapy has delayed the onset of complications associated with T1D.
Research, such as the studies conducted under the DCCT/EDIC programs, has demonstrated that maintaining consistent glycemic control significantly reduces the negative health impacts on quality of life. However, complications such as retinopathy, neuropathy, and psychological issues like depression remain substantial barriers to effective management.
These findings underscore the importance of holistic treatment approaches that address glycemic control and the psychological and functional dimensions of living with diabetes.
Providing comprehensive support, early intervention, and open communication about sensitive topics such as sexual and urologic health can help patients navigate the complexities of long-term diabetes care, ultimately improving their quality of life despite these challenges.