AI Contribution
At HealthSpectra, we may use AI to refine grammar and structure, but every piece is shaped, checked, and approved by real people, our expert writers and editors, to ensure clarity, credibility, and care. Learn more..Affiliate Disclaimer
Some links in this article are affiliate links. We may earn a small commission if you make a purchase through these links, at no extra cost to you. We only recommend products we find useful to our readersType 1 diabetes, or T1D, is a challenging condition that requires day-to-day management and modifications in lifestyle. It tends to affect almost every aspect of daily life and, when left untreated, can cause fatal complications.
This article covers the most critical aspects of T1D, such as diagnosis, management techniques, signs and symptoms, and potential long-term complications.
How Type 1 Diabetes Develops
Type 1 diabetes is an autoimmune disease in which the pancreas’s β-cells responsible for insulin production are destroyed. The immune system, specifically T-cells, mistakenly attacks and destroys these β-cells, which results in a deficiency of insulin.
Without enough insulin, glucose from the blood cannot enter cells efficiently, leading to high blood glucose levels or hyperglycemia. The exact trigger for this autoimmune response is not clearly understood, but genetic and environmental factors play significant roles.
Genetic predisposition can be identified through markers such as human leukocyte antigen (HLA) genes, particularly DQA and DQB, strongly linked to increased susceptibility to T1D. Moreover, specific environmental triggers such as viral infections, diet, or stress might initiate or accelerate the autoimmune process.
The progression of type 1 diabetes varies among individuals. In some cases, the β-cell destruction is rapid, especially in children and adolescents, while in others, the decline is slower, sometimes taking years before significant symptoms appear.
The course of type 1 diabetes is variable. In some, the β-cell destruction is rapid, particularly in children and adolescents, whereas in others, the decline is slower, sometimes taking years before significant symptoms develop.
Also Read: Content_Glucose Absorption in Children vs. Adults with Diabetes
During the disease progression, autoantibodies against insulin, glutamic acid decarboxylase (GAD), and other pancreatic proteins are often present, which can be early disease markers even before hyperglycemia is clinically apparent.
In the initial stages, symptoms are usually mild. However, when more β-cells are destroyed, and the production of insulin is critically low, patients may present with more severe symptoms, like weight loss, excessive thirst (polydipsia), frequent urination (polyuria), and fatigue.
If left untreated, the lack of insulin can cause ketoacidosis, a potentially life-threatening condition where fat metabolism creates ketones, which are too acidic for the blood.
Symptoms of Type 1 Diabetes

Type 1 diabetes (T1D) presents with a variety of symptoms that arise from an elevated blood glucose level as a result of inadequate insulin production. Early recognition of these symptoms is essential for timely diagnosis and management.
Symptoms may develop quickly, often within a few days or weeks, especially in children and adolescents. Common symptoms include:
1. Increased Thirst (Polydipsia)
Excessive thirst is one of the first signs of T1D. As blood glucose levels rise, the body tries to dilute excess sugar by pulling water from tissues. This results in dehydration and an intense urge to drink liquids.
2. Frequent Urination (Polyuria)
Increased thirst leads to increased fluid intake, which results in frequent urination. The kidneys work to excrete excess glucose, and as glucose spills into the urine, it draws more water with it, leading to urination that occurs more often than usual.
3. Extreme Hunger (Polyphagia)
Despite consuming more calories than normal, people with T1D feel hungry because the body fails to absorb glucose. With insufficient insulin, glucose cannot penetrate the cells and gain energy, which usually causes an individual to crave more food.
4. Unexplained Weight Loss
Even though there is hunger and eating, a patient with T1D experiences weight loss. This results from the breakdown of fatty tissues and muscles used to gain energy, as glucose will not be available for cells.
5. Fatigue
Glucose cannot enter cells due to the body’s inability to produce enough insulin, limiting the energy supply. This presents with weakness and fatigue, as the body is unable to use its energy effectively.
6. Blurred Vision
High blood sugar can cause fluid to be pulled from the lenses of the eyes, affecting the eye’s ability to focus. This symptom may improve with better blood sugar control.
7. Slow-healing sores and Frequent Infections
High blood glucose can impair the body’s ability to heal wounds and fight infections. People with T1D may notice slower cut healing and an increased frequency of infections.
8. Diabetic Ketoacidosis (DKA)
In some instances, T1D may have symptoms of diabetic ketoacidosis. This serious condition arises when the body breaks down fat for fuel, producing ketones that can accumulate to dangerous levels. Symptoms of DKA include nausea, vomiting, abdominal pain, confusion, and a fruity odor on the breath.
Causes and Risk Factors
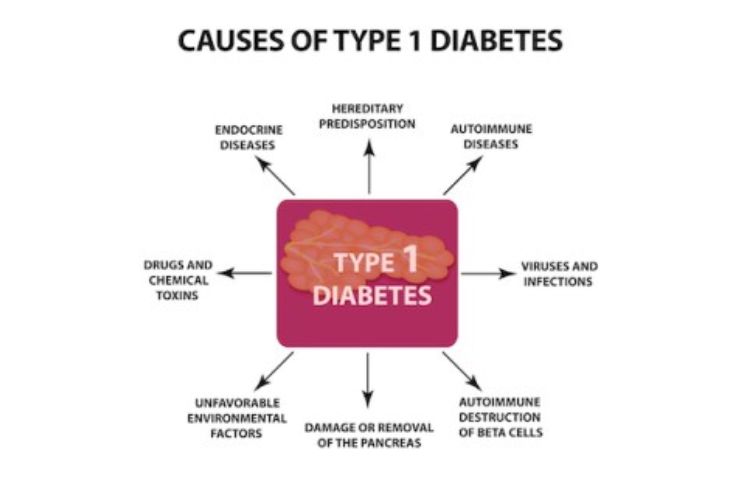
The exact reason for this autoimmune response has not been known, yet several factors are thought to contribute to its development. Below are the major causes listed. You may find out the risk factors in this detailed article.
- Genetic Factors
- Autoimmune Triggers
- Environmental Triggers
Diagnosis of Type 1 Diabetes
Diagnosis combines medical history reviews, physical examination, and specific blood investigations to estimate or evaluate the glucose content present in the blood. Timely and correct detection helps ensure proper disease management.
Also Read: Content_What is Type 1 Diabetes? An Introduction
Potential Complications of Type 1 Diabetes
Type 1 diabetes can cause a lot of short-term and long-term complications if not handled appropriately. These complications usually come from the prolonged time the blood is maintained at high glucose levels.
This can damage blood vessels and nerves found throughout the body. Awareness and proper management are necessary to help mitigate these risks.
Also Read: Content_The Science Behind Type 1 Diabetes: How It Affects the Body
Living with Type 1 Diabetes

Living with type 1 diabetes is challenging and requires constant management to maintain health and well-being. The diagnosis is often overwhelming, but most individuals learn to manage their lives effectively with the right strategies and support.
1. Daily Management
Effective management of T1D involves several key components:
- Blood Sugar Monitoring: Continuously monitoring blood glucose is important to understand what different foods, activities, and insulin doses do for blood sugar levels. For instance, CGMs would give real-time data regarding blood sugar levels throughout the day.
- Insulin Therapy: Since T1D requires lifelong insulin therapy, individuals need to develop a routine for insulin administration through injections or insulin pumps. Understanding how to adjust insulin doses based on carbohydrate intake, activity level, and stress is crucial for effective management.
- Healthy Eating: Adequate nutrient intake is an essential management tool for blood glucose levels. A person with T1D should focus on the amount of whole foods, including all types of fruits and vegetables, whole grains, lean protein, and healthy fats, as a source of calories. Counting carbs or estimating what will raise blood glucose makes meal planning easier.
- Physical Activity: Exercise can contribute to better blood sugar management. Still, to avoid hypoglycemia, one has to regulate blood sugar levels both before, during, and after exercise. An individual should devise a strategy to manage insulin and food while exercising.
2. Emotional and Social Aspects
Living with T1D can also impact emotional well-being and social interactions:
- Support Networks: Connecting with other T1D sufferers can provide emotional support and valuable advice. In-person diabetes support groups and online diabetes communities can provide a sense of community and understanding.
- Mental Health: Those with T1D experience anxiety, depression, or diabetes distress. Professional mental health care from chronic illness-educated professionals can be beneficial to cope with those feelings.
- Education and Advocacy: It is important to be educated about T1D and advocate for oneself in healthcare settings. Education about the condition, treatment options, and emerging research can empower individuals to make informed decisions about their health.
3. Navigating Life Events
Certain life events may pose additional challenges for those with T1D:
- Traveling: Pre-travel planning must consider the storage of insulin, choice of meals, and blood sugar monitoring. Carrying a diabetes kit with supplies and snacks is essential for managing diabetes when on the go.
- School and Work: Individuals with T1D may need to inform teachers, employers, and coworkers of their needs. A management plan that details how to handle blood sugar checks and insulin administration can help create a supportive environment.
- Holidays and Special Occasions: Celebrating holidays or special events may involve navigating food choices and maintaining blood glucose levels. Planning and finding ways to enjoy festivities while managing T1D can contribute to a positive experience.
Conclusion
Type 1 diabetes is a challenging condition that requires lifelong management and care. Understanding its development, symptoms, causes, diagnosis, possible complications, and strategies for everyday living empowers the person to take control of his or her health.
Of course, the journey does not come without obstacles; advances in diabetes care and support systems make invaluable resources for those with T1D.
With constant studies and education, there is hope that people suffering from type 1 diabetes will have fewer challenges. By encouraging active management of type 1 diabetes, interaction with support networks, and advocacy for health, a life filled with hope and positivity will flourish.
Achieving health and well-being requires embracing a balanced lifestyle and maintaining open communication with healthcare providers.
In this Article